https://doi.org/10.55788/e7bc440c
Prof. Arnon Kater (Amsterdam University Medical Center, the Netherlands) presented the outcomes of the open-label, single arm, phase 3b VENICE 1 trial. The purpose of this study was to evaluate the efficacy of venetoclax monotherapy in participants with R/R CLL, including those with the 17p deletion, TP53 mutation, or those who have received prior treatment with a BCRi.
The primary endpoint of the study was complete remission (CR) rate or CR with incomplete bone marrow recovery (CRi) in BCRi-naïve patients at week 48. Key secondary endpoints were overall response rate (ORR), progression-free survival (PFS), overall survival (OS), quality of life (QOL) assessed via Functional Assessment of Cancer Therapy – Leukemia Questionnaire (FACT-Leu), and safety. Minimal residual disease (MRD) levels were set as an exploratory endpoint.
Patients (n=258) underwent a 5-week ramp-up from 20 mg to 400 mg venetoclax daily, and then stayed on 400 mg for 2 years. Clinical response was assessed (iwCLL 2008) at weeks 24, 36, and 48. Most patients were BCRi-naïve (n=191), but 67 had had prior BCRi-treatment (BCRi-exposed). Site-reported genetics indicated that 17p-loss or TP53 mutation was present in 16.8% of BCRi-naïve patients versus 43.3% of BCRi-exposed patients.
The primary endpoint was met; at week 48, CR/CRi rates were 35.1% in the BCRi-naïve cohort as opposed to 25.4% in the BCRi-exposed group (see Table). ORR was 85.3% for BCRi-naïve patients compared with 64.2% in the BCRi-exposed group. Furthermore, MRD at week 48 was undetectable in 35.6% of the BCRi-naïve patients and 26.9% of the BCRi-exposed patients. PFS was 30.5 months (77.0%) overall, 28.6 months (67.1%) in patients with 17p/TP53 aberration, and 30.5 months (79.4%) versus 28.6 months (69.9%) for the BCRi-naïve and BCRi-exposed groups, respectively. Median PFS was not reached for patients who had either undetectable MRD or CR/CRi, suggestive of a deep and durable response. PFS with partial remission/nodular partial remission was 30.5 months. OS was 83.7% overall, 88.0% for BCRi-naïve patients, and 71.6% for BCRi-exposed patients. QOL showed clinically meaningful improvement at week 48 for all subgroups.
Table. Response rates with VEN treatment in BCRi-naïve and BCRi-experienced groups

BCRi, B-cell receptor pathway inhibitors; CI, confidence interval; CR, complete response; CRi, complete response with incomplete bone marrow recovery; MRD, minimal residual disease; nPR, nodular partial remission; ITT, intention to treat; PB, peripheral blood; PR, partial remission; uMRD, undetectable minimal residual disease; VEN, venetoclax.
*Median OS was not reached.
Toxicity was high, but manageable; 74.4% experienced grade ≥3 adverse events (AEs) (neutropenia 37.2%, infection 19.0%); 12.4% of patients reduced dose due to AEs, and 109 (42.2%) discontinued venetoclax (12.8% because of AEs, 10.9% because of disease progression). No new safety signals were observed.
In brief, venetoclax monotherapy can achieve deep responses (CR, undetectable MRD) and has a tolerable and manageable safety profile in patients with R/R CLL.
- Kater A, et al. Efficacy of venetoclax in patients with relapsed/refractory chronic lymphocytic leukemia: primary endpoint analysis of the international phase 3b trial (VENICE I). EHA25 Virtual, 11-21 June 2020, Abstract S156.
Posted on
« MRD assessment post-CAR-T predicts ALL allo-HSCT bridging Next Article
Zanubrutinib versus ibrutinib in Waldenström macroglobulinaemia »
Table of Contents: EHA 2020
Featured articles
Myeloid
VIALE-A: newly diagnosed chemo-ineligible AML
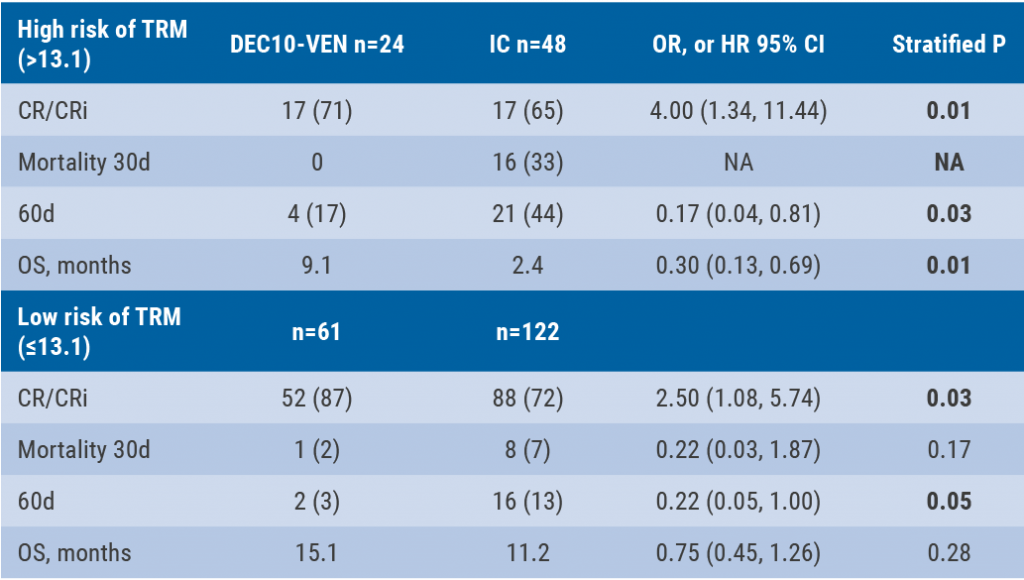
DEC10-VEN superior to intensive chemotherapy in high-risk AML
Magrolimab plus azacitidine: good ORR in MDS/AML
Asciminib monotherapy in Ph+ CML: major molecular responses
CML TKI interruption: Swedish registry results
Patients with lower-risk MDS benefit from imetelstat
Better outcomes adding enasidenib to azacitidine in mIDH2-AML
Lymphoid
PET-stratification can omit radiotherapy in early-stage unfavourable Hodgkin lymphoma
Pembrolizumab improves PFS for relapsed/refractory Hodgkin lymphoma
Promising first-in-human trial of epcoritamab in B-NHL
Two trials: acalabrutinib in CLL
Zanubrutinib versus ibrutinib in Waldenström macroglobulinaemia
Deep responses in R/R CLL with venetoclax monotherapy
MRD assessment post-CAR-T predicts ALL allo-HSCT bridging
Plasma Cell Dyscrasias
Daratumumab for light-chain amyloidosis
Isatuximab triplet improves PFS in R/R MM
Initial results from CAR-T cell therapy in MM: KarMMa
Graft-Versus-Host Disease
GRAVITAS-301: improved complete aGVDH response
Ruxolitinib improves steroid-refractory aGVHD across subtypes
Benign Haematology
Paroxysmal nocturnal haemoglobinuria treatment with pegcetacoplan
Mitapivat, a pyruvate kinase-R activator, in SCD is safe with early efficacy results
SCD LentiGlobin gene therapy: new data on VOC and ACS
Paediatric Haematology
Venetoclax + navitoclax promising for R/R ALL or LL
Nivolumab/brentuximab vedotin in R/R HL: good CMR rates
Bench-to-Bedside Science from the Presidential Symposium
Microbiome predicts B-ALL predisposition
Netrin-1 regulates haematopoietic stem cells
Unrecognised role of iron in neutrophil differentiation
Related Articles
DEC10-VEN superior to intensive chemotherapy in high-risk AML
GRAVITAS-301: improved complete aGVDH response
Endothelial damage in COVID-19
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

