https://doi.org/10.55788/c838601b
The new guideline was developed by the task force for the diagnosis and treatment of pulmonary hypertension of the ESC and the ERS [1–3]. Prof. Stephan Rosenkranz (Heart Center at the University Cologne, Germany) pointed out that patient representatives were actively involved for the first time.
PH is not a rare condition as it affects 1% of the global and 10% of the elderly population. The clinical classification of PH in 5 groups was maintained in the novel guideline, with only minor changes. “When assessing patients, it is of utmost importance to find the right diagnosis, because therapy is different,” Prof. Rosenkranz stressed. In the new guideline, there are minor changes in the haemodynamic definition of PH, for example:
- The threshold of PH was lowered to a mean pulmonary arterial pressure (mPAP) >20 mmHg
- The threshold of pre-capillary PH was lowered to a pulmonary vascular resistance (PVR) >2 Woods units (WU)
- The threshold of isolated post-capillary PH was lowered to a PVR ≤2 WU
- The threshold of combined post- and pre-capillary PH was lowered to a PVR >2 WU.
New diagnostic algorithm aims at earlier detection
The statement contains a new definition of exercise PH, in case the mPAP/cardiac output slope between rest and exercise is >3 mmHg/L/min.
“In the new guideline, the diagnostic algorithm has been re-structured. Importantly, a fast-track referral in case of warning signs is included,” Prof. Rosenkranz said.
The general practitioner plays a key role in patients with unexplained dyspnoea and/or suspicion of PH. They can perform a general assessment (see Figure) and according to the suspected cause (lung disease, PH, or cardiac disease) the patient is referred to a cardiologist or a pulmonologist.
Figure: Step 1 of the novel diagnostic algorithm of patients with unexplained exertional dyspnoea and/or suspected PH [2]

In step 2 of the diagnostic algorithm a more comprehensive assessment of the heart and lung is performed. In step 3, in case of a high PH probability, referral to a PH centre for invasive assessment and comprehensive PH work-up is suggested. At any time, a fast-track referral to a PH centre in case of warning signs or when pulmonary arterial hypertension (PAH) and chronic thrombo-embolic pulmonary hypertension (CTEPH) are suspected is recommended.
The new guideline presents far more details in transthoracic echocardiographic parameters in the assessment of PH. The presence of risk factors for PAH moves the patient up 1 category in the PH probability. “We added the ratio of tricuspid annular plane systolic excursion and systolic pulmonary arterial pressure (TAPSE /sPAP) as a sensitive marker to diagnose PH”; Prof. Rosenkranz explained. A TAPSE/sPAP ratio of <0.55 mm/mmHg in the echocardiography is suggestive of pulmonary hypertension. Right heart catheterisation remains gold standard to diagnose PH.
Modified PAH treatment algorithm with a focus on cardiopulmonary comorbidity
Prof. Marion Delcroix (University Hospitals Leuven, Belgium) presented the part of group 1 of the clinical classification, patients with PAH. The haemodynamic definition of PAH implies a PVR >2 WU and pulmonary arterial wedge pressure (PAWP) ≤15 mm Hg.
Once the diagnosis is confirmed, a comprehensive risk assessment in PAH in a 3-strata model is recommended in the new guideline. “The single components of low risk, intermediate risk, and high risk did not change, but the NT-proBNP threshold was adjusted,” Prof. Delcroix said.
The PAH treatment algorithm has been modified, highlighting the importance of cardiopulmonary comorbidities. In case of a confirmed diagnosis at a PH centre initial monotherapy with PDE5 inhibitors or endothelin receptor antagonists is recommended in patients with cardiopulmonary comorbidities, whereas all other patients benefit from a combination of these agents.
At follow up, a novel simplified 4-strata risk-assessment tool is recommended as a basic risk-stratification tool.
PH associated with left heart disease (LHD): the most frequent subgroup.
Prof. Rosenkranz also explained novel recommendations in group 2 of the clinical classification, PH associated with left heart disease (LHD), the most frequent subgroup. There are new recommendations for right heart catheterisation in patients with suspected PH and LHD – if it aids in the management decision – and in patients with severe tricuspid regurgitation (± LHD) prior to surgical or interventional valve repair.
Regarding therapy, there are 2 new class I recommendations:
- In patients with LHD and combined post- and pre-capillary PH with a severe pre-capillary component, an individualised approach to treatment is recommended
- When patients with PH and multiple risk factors for LHD, who have a normal PAWP at rest but an abnormal response to exercise or fluid challenge, are treated with PAH drugs, close monitoring is recommended
Prof. Delcroix then presented the part of PH associated with lung disease, group 3 of the clinical classification and a common cause of PH. For the first time, there is a recommendation for PH medical therapy in group 3, based on a single positive study: inhaled treprostinil may be considered in PH associated with interstitial lung disease (ILD).
PDE5 inhibitors may be considered in patients with severe PH associated with ILD (individual decision-making in PH centres), but is not recommended in patients with ILD and non-severe PH.
Multi-modality approach warranted in chronic thromboembolic PH
For chronic thromboembolic PH (CTEPH; group 5) there is an overlap in surgical/invasive procedures and medical therapy.
In a new diagnostic algorithm for symptomatic CTEPH patients, perfusion imaging and echocardiography is recommended. In case there are signs of PH, referral to a CTEPH/PH centre is recommended.
“In a patient with confirmed CTEPH, lifelong therapeutic anticoagulation is recommended,” Prof. Delcroix explained.
In case patients are operable, pulmonary endarterectomy is the treatment of choice. If this is not possible, patients will receive medical therapy. The same is true for patients with persistent/recurrent PH after pulmonary endarterectomy. Riociguat is recommended for symptomatic patient with inoperable CTEPH or with persistent/recurrent PH after pulmonary endarterectomy (class I).
Finally, medical therapy should be considered prior to the intervention in patients with CTEPH who are candidates for balloon pulmonary angioplasty. The last part of the guidelines outlines requirements for a PH centre.
- Presentations in Session: “2022 ESC Guidelines Overview”, ESC Congress 2022, Barcelona, Spain, 26–29 August.
- Presentations in Session: “2022 ESC-ERS Guidelines for the diagnosis and treatment of pulmonary hypertension”, ESC Congress 2022, Barcelona, Spain, 26–29 August.
- Humbert M, et al. Eur Heart J. 2022 Aug 26;ehac237. doi: 10.1093/eurheartj/ehac237. Online ahead of print.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Cardiovascular assessment and management of patients undergoing non-cardiac surgery Next Article
New and first ESC cardio-oncology guideline »
« Cardiovascular assessment and management of patients undergoing non-cardiac surgery Next Article
New and first ESC cardio-oncology guideline »
Table of Contents: ESC 2022
Featured articles
ESC Clinical Practice Guidelines
Prevention of VT and sudden cardiac death: the new recommendations
New and first ESC cardio-oncology guideline
The 2022 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension
Cardiovascular assessment and management of patients undergoing non-cardiac surgery
Heart Failure
Old dogs, new tricks: Acetazolamide plus loop diuretics improves decongestion
No effect of neprilysin inhibition on cognition
Dapagliflozin DELIVERs for HFmrEF/HFpEF
Meta-analysis of DELIVER and EMPEROR-Preserved
Anticoagulation
Rheumatic heart disease-associated AF: standard-of-care holds ground
New anticoagulant safe and maybe effective: PACIFIC-AMI and PACIFIC-Stroke outcomes
AXIOMATIC-SSP: Reducing risk of ischaemic stroke with factor XIa inhibition?
Evolving evidence for P2Y12 inhibition in chronic coronary syndromes: PANTHER
Prevention
Danish study suggests starting CVD screening before age 70
Polypill SECUREs win in secondary prevention in elderly
Long-term therapy with evolocumab associated with lower CV mortality
ARBs + beta-blockers may delay Marfan syndrome aortic root replacement
ENTRIGUE: Subcutaneous pegozafermin in severe hypertriglyceridaemia
Artificial Intelligence & Digital Health – What Is New
First RCT evidence for use of AI in daily practice
AI-enhanced echography supports aortic stenosis patients
Ischaemia
Medical therapy versus PCI for ischaemic cardiomyopathy
Allopurinol disappoints in ALL-HEART
Conservative or invasive management for high-risk kidney disease patients with ischaemia?
Genotype-guided antiplatelet therapy in patients receiving PCI
Other HOTLINE Sessions
BOXing out oxygen and blood pressure targets
Coronary CT angiography diagnostics compared head-to-head
High-dose influenza vaccine: mortality benefit?
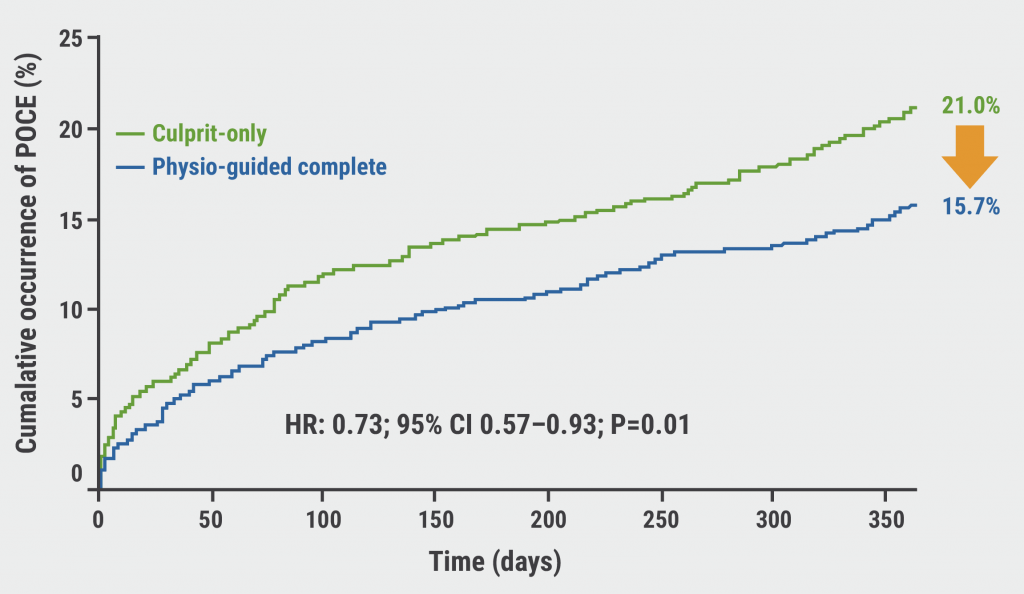
FFR-guided decision-making in patients with AMI and multivessel disease
Related Articles
September 8, 2020
TWILIGHT sub-study: same outcomes for diabetes patients
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

