https://doi.org/10.55788/65be7341
Patients with ischaemic cardiomyopathy continue to have high rates of mortality and hospitalisation for heart failure even with contemporary medical and device therapy. Previously, the STICHES trial has shown that revascularisation can improve the 10-year outcomes in this vulnerable patient population [1]. The REVIVED-BCIS2 trial (n=700; NCT01920048) sought to conclusively define the added value of PCI (n=353) over optimal medical therapy (n=353) in the first randomised trial in this population. The results were presented by Prof. Divaka Perera (Guy's & St Thomas' NHS Foundation Trust, London, UK) and were simultaneously published in the New England Journal of Medicine [2,3].
The primary composite endpoint of all-cause death or heart failure hospitalisation was not met: 37.2% of the PCI group experienced a primary endpoint event compared with 38% of the group on optimal medical treatment (HR 0.99; 95% CI 0.78–1.27; P=0.96), over a median of 3.4 years of follow-up. The treatment effect was consistent across all subgroups. There were also no significant differences in LVEF at 6 and 12 months.
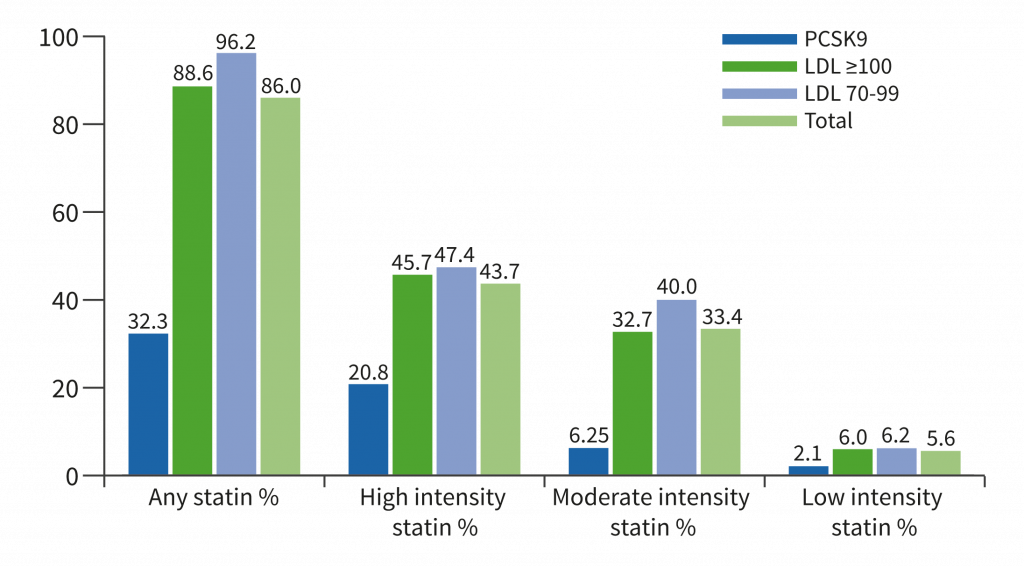
Quality-of-life scores favoured PCI at the 6-month and 12-month timepoints, but the curves narrowed over time with medical therapy, and this advantage disappeared by 2 years, indicating that this benefit was not sustained (see Figure).
Figure: REVIVED major secondary endpoint was health-related quality-of-life (KCCQ score), which showed early differences, but the gap was not sustainable over time [2]

OMT, optimal medical therapy; PCI, percutaneous coronary intervention
- Velazquez EJ, et al. N Engl J Med. 2016 Apr 21;374(16):1511-20.
- Perera D, et al. REVIVED - Percutaneous Revascularisation for Ischaemic Ventricular Dysfunction. Hot Line Session 3, ESC Congress 2022, Barcelona, Spain, 26–29 August.
- Perera D, et al. N Engl J Med. 2022 Aug 27. doi: 10.1056/NEJMoa2206606.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Allopurinol disappoints in ALL-HEART Next Article
Smartphones for AF detection »
« Allopurinol disappoints in ALL-HEART Next Article
Smartphones for AF detection »
Table of Contents: ESC 2022
Featured articles
ESC Clinical Practice Guidelines
Prevention of VT and sudden cardiac death: the new recommendations
New and first ESC cardio-oncology guideline
The 2022 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension
Cardiovascular assessment and management of patients undergoing non-cardiac surgery
Heart Failure
Old dogs, new tricks: Acetazolamide plus loop diuretics improves decongestion
No effect of neprilysin inhibition on cognition
Dapagliflozin DELIVERs for HFmrEF/HFpEF
Meta-analysis of DELIVER and EMPEROR-Preserved
Anticoagulation
Rheumatic heart disease-associated AF: standard-of-care holds ground
New anticoagulant safe and maybe effective: PACIFIC-AMI and PACIFIC-Stroke outcomes
AXIOMATIC-SSP: Reducing risk of ischaemic stroke with factor XIa inhibition?
Evolving evidence for P2Y12 inhibition in chronic coronary syndromes: PANTHER
Prevention
Danish study suggests starting CVD screening before age 70
Polypill SECUREs win in secondary prevention in elderly
Long-term therapy with evolocumab associated with lower CV mortality
ARBs + beta-blockers may delay Marfan syndrome aortic root replacement
ENTRIGUE: Subcutaneous pegozafermin in severe hypertriglyceridaemia
Artificial Intelligence & Digital Health – What Is New
First RCT evidence for use of AI in daily practice
AI-enhanced echography supports aortic stenosis patients
Ischaemia
Medical therapy versus PCI for ischaemic cardiomyopathy
Allopurinol disappoints in ALL-HEART
Conservative or invasive management for high-risk kidney disease patients with ischaemia?
Genotype-guided antiplatelet therapy in patients receiving PCI
Other HOTLINE Sessions
BOXing out oxygen and blood pressure targets
Coronary CT angiography diagnostics compared head-to-head
High-dose influenza vaccine: mortality benefit?
FFR-guided decision-making in patients with AMI and multivessel disease
Related Articles
October 27, 2022
Genotype-guided antiplatelet therapy in patients receiving PCI
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

