https://doi.org/10.55788/2c8e8275
The DANCAVAS study (ISRCTN12157806) was a population-based, randomised-controlled screening trial attempting to address the significant increase in the average life expectancy and incipient CVD, explained Prof. Axel Cosmus Pyndt Diederichsen (Odense University Hospital, Denmark) in his presentation [1]. The results were simultaneously published in the New England Journal of Medicine [2]. The trial aimed to evaluate the health benefits and cost effectiveness of using non-contrast CT scans to measure coronary artery calcification and identify aortic/iliac aneurysms and measurements of the ankle brachial blood pressure index as part of a multifocal screening and intervention program for CVD in men aged 65–74.
Between September 2014 and September 2017, 46,526 Danish men aged 65–74 years living in particular municipalities of Denmark were included; no exclusion criteria were applied. One third (n=16,736) of the men were randomised to receive an invitation to the screening, while the remaining two thirds (n=29,790) of the men acted as clinical controls. The primary endpoint was all-cause mortality. Key secondary endpoints were stroke, myocardial infarction (MI), amputation due to vascular disease, aortic dissection, and aortic rupture. The researchers powered the trial with the assumption that the attendance to screening would be 70%.
However, the attendance to screening was only 63%, and the primary endpoint was not met. With a median follow-up of 5.6 years, 12.6% men in the screening group and 13.1% men in the control group had died, corresponding to a non-significant 5% relative risk reduction (HR 0.95; 95% CI 0.90–1.00; P=0.062). To prevent a single death, the number needed to invite to screening was 155.
Subgroup analyses did indicate that a slightly younger age group (65–69 years) may benefit from screening; while there was no difference among men aged 70 years and older (HR 1.01; 95% CI 0.94–1.09; P=0.747), an 11% decreased risk in those aged 65–69 years was observed (HR 0.89; 95% CI 0.83–0.96; P=0.004).
Secondary endpoint results varied. For stroke, 7.0% men in the screening group experienced a stroke compared with 7.5% in the control group (HR 0.93; 95% CI 0.86–0.99; P=0.035). There were no differences between the 2 groups in aortic dissection (HR 0.95; 95% CI 0.61–1.49; P=0.827), aortic rupture (HR 0.81; 95% CI 0.49–1.35; P=0.420), amputation due to vascular disease (HR 1.05; 95% CI 0.80–1.38; P=0.711), or MI (HR 0.91; 95% CI 0.81–1.03; P=0.134).
Not surprisingly, the group who had attended screening were prescribed more lipid-lowering agents (20.7% vs 9.0%; HR 2.54; 95% CI 2.42–2.67; P<0.001), and antithrombotic agents (22.9% vs 8.3%; HR 3.12; 95% CI 2.97–3.28; P<0.001). Likewise, elective aortic aneurysm repair was more common in the screening group compared with the control group (1.5% vs 1.2%; HR 1.29; 95% CI 1.07–1.48; P=0.006). However, there were no differences in prescription of anticoagulants, antihypertensive medications, or therapies to treat diabetes.
Prof. Diederichsen concluded optimistically: “We observed a substantial reduction in the combined endpoint of death, stroke, or MI in elderly men by comprehensive cardiovascular screening. Our results point quite firmly at a screening target age below 70 years.”
- Diederichsen ACP, et al. DANCAVAS - Screening and intervention to prevent cardiovascular disease. Hot Line Session 2, ESC Congress 2022, Barcelona, Spain, 26–29 August.
- Lindholt JS, et al. N Engl J Med. 2022;387:1385-1394.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Polypill SECUREs win in secondary prevention in elderly Next Article
Evolving evidence for P2Y12 inhibition in chronic coronary syndromes: PANTHER »
« Polypill SECUREs win in secondary prevention in elderly Next Article
Evolving evidence for P2Y12 inhibition in chronic coronary syndromes: PANTHER »
Table of Contents: ESC 2022
Featured articles
ESC Clinical Practice Guidelines
Prevention of VT and sudden cardiac death: the new recommendations
New and first ESC cardio-oncology guideline
The 2022 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension
Cardiovascular assessment and management of patients undergoing non-cardiac surgery
Heart Failure
Old dogs, new tricks: Acetazolamide plus loop diuretics improves decongestion
No effect of neprilysin inhibition on cognition
Dapagliflozin DELIVERs for HFmrEF/HFpEF
Meta-analysis of DELIVER and EMPEROR-Preserved
Anticoagulation
Rheumatic heart disease-associated AF: standard-of-care holds ground
New anticoagulant safe and maybe effective: PACIFIC-AMI and PACIFIC-Stroke outcomes
AXIOMATIC-SSP: Reducing risk of ischaemic stroke with factor XIa inhibition?
Evolving evidence for P2Y12 inhibition in chronic coronary syndromes: PANTHER
Prevention
Danish study suggests starting CVD screening before age 70
Polypill SECUREs win in secondary prevention in elderly
Long-term therapy with evolocumab associated with lower CV mortality
ARBs + beta-blockers may delay Marfan syndrome aortic root replacement
ENTRIGUE: Subcutaneous pegozafermin in severe hypertriglyceridaemia
Artificial Intelligence & Digital Health – What Is New
First RCT evidence for use of AI in daily practice
AI-enhanced echography supports aortic stenosis patients
Ischaemia
Medical therapy versus PCI for ischaemic cardiomyopathy
Allopurinol disappoints in ALL-HEART
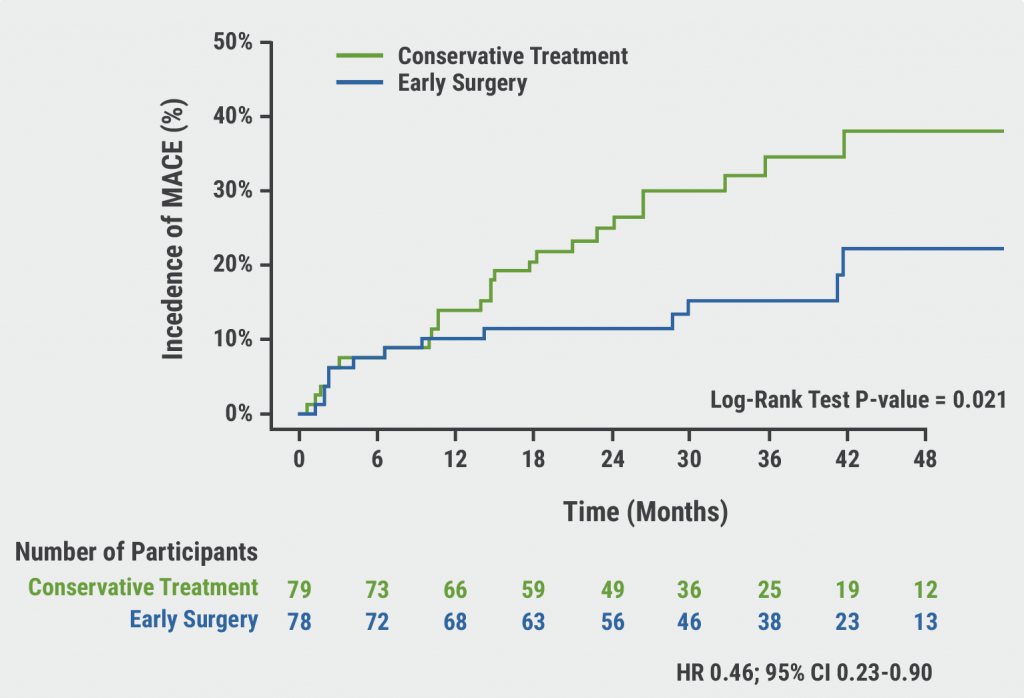
Conservative or invasive management for high-risk kidney disease patients with ischaemia?
Genotype-guided antiplatelet therapy in patients receiving PCI
Other HOTLINE Sessions
BOXing out oxygen and blood pressure targets
Coronary CT angiography diagnostics compared head-to-head
High-dose influenza vaccine: mortality benefit?
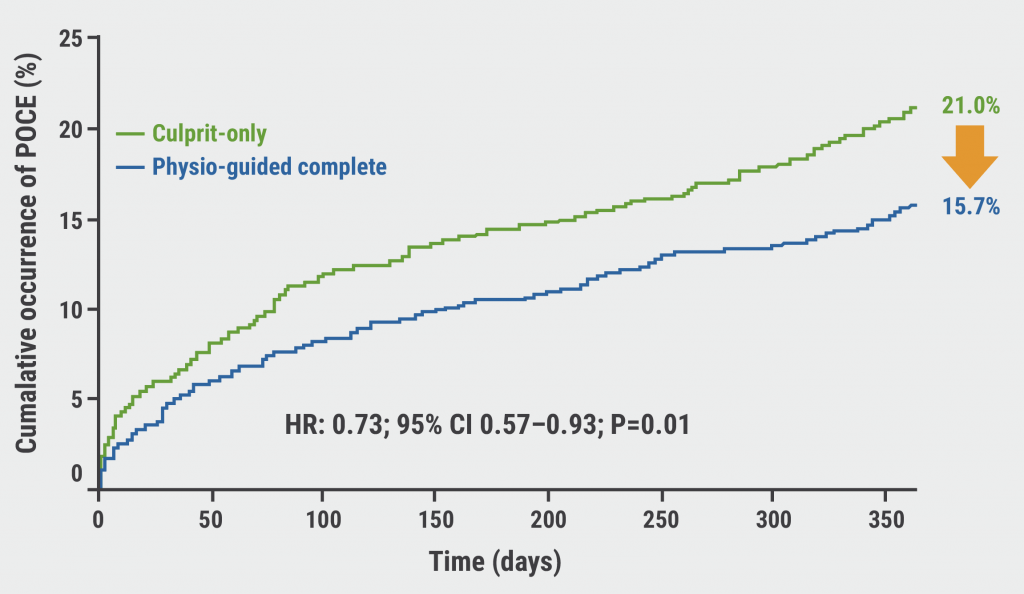
FFR-guided decision-making in patients with AMI and multivessel disease
Related Articles
October 27, 2022
Danish study suggests starting CVD screening before age 70
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

