https://doi.org/10.55788/44b11740
“Although hypertensive disorders of pregnancy are associated with an increased risk of cardiovascular disease, there are no proven therapies to reduce the post-partum risk,” according to Dr Jamie Kitt (University of Oxford, UK) [1]. The POP-HT study (NCT04273854) randomised 220 women with gestational hypertension or pre-eclampsia 1:1 to standard NHS care in the control group or the intervention arm, in which self-monitored BP readings were sent to a physician who subsequently optimised BP medication for the respective participants [1,2]. The primary endpoint was the 24-hour mean diastolic BP at approximately 9 months post-partum.
At 9 months post-partum, the between-group difference in 24-hour mean diastolic BP was -5.8, favouring the intervention arm over the control arm (95% CI -4.2 to -7.4) [1]. Likewise, the difference in 24-hour mean systolic BP was -6.5 mmHg, favouring the intervention arm (95% CI -4.2 to -8.8). “Furthermore, there were 29 BP-related re-admissions in the control arm versus 8 in the intervention arm, meaning that we need to treat 5 individuals to avoid 1 BP-related post-natal re-admission,” added Dr Kitt.
According to Dr Kitt, the results of this trial are clinically meaningful. “A 5 mmHg improvement in BP would result in a 20% reduction in lifetime cardiovascular risk if this improvement is maintained in the long-term,” he concluded [1,2].
- Kitt J, et al. Physician optimized postpartum hypertension treatment (POP-HT) randomised trial. LB04, AHA Scientific Sessions 2023, 11–13 November, Philadelphia, USA.
- Kitt J, et al. J. Am. Med. Assoc. 2023;330(20):1991–1999.
Copyright ©2024 Medicom Medical Publishers
Posted on
Previous Article
« Biannual zilebesiran associated with substantial BP reductions Next Article
Intensive BP intervention reduces risk of dementia »
« Biannual zilebesiran associated with substantial BP reductions Next Article
Intensive BP intervention reduces risk of dementia »
Table of Contents: AHA 2023
Featured articles
Abelacimab substantially lowers bleeding risk compared with rivaroxaban
Hot Topics in CAD/PAD
MINT: Liberal or restrictive transfusion strategy in MI with anaemia?
ORBITA-2 confirms PCI effective for symptom relief in patients with stable angina
Nicotinamide riboside shows promising trend for walking function in PAD
Pemafibrate reduces microvascular complications of PAD and T2D
Dapagliflozin improves cardiometabolic outcomes in myocardial infarction
Optimising Hypertension Outcomes
Edoxaban versus warfarin in chronic thromboembolic pulmonary hypertension
Sodium intake and blood pressure: new insights
Post-partum intervention lowers BP after hypertensive pregnancy
Biannual zilebesiran associated with substantial BP reductions
Future of Lipid-Lowering Therapies
Encouraging data for lepodisiran as Lp(a) lowering therapy
Gene editing may change the treatment landscape of hypercholesterolaemia
REPRIEVE: Mechanisms behind MACE reduction in HIV population on pitavastatin
Recaticimab may offer a solution for uncontrolled hypercholesterolaemia
Atrial Fibrillation and Sudden Cardiac Death
Abelacimab substantially lowers bleeding risk compared with rivaroxaban
Liraglutide may improve post-ablation outcomes in obese patients with AF
Single or dual cardioversion in patients with obesity and AF?
NOAH-AFNET 6: Does the duration of AHRE influence response to edoxaban?
ARTESIA: How useful is anticoagulation in subclinical AF?
Jewel IDE: High compliance rates for novel patch wearable cardioverter defibrillator
Sudden cardiac death in athletes: incidence, causes, and trends over 20 years
Miscellaneous Trials
Successful results for semaglutide in the highly anticipated SELECT trial
Can a walking intervention improve functional status and quality of life in HFrEF?
Head-to-head: Surgical embolectomy versus ultrasound-assisted thrombolysis in high-risk pulmonary embolism
Related Articles
October 30, 2023
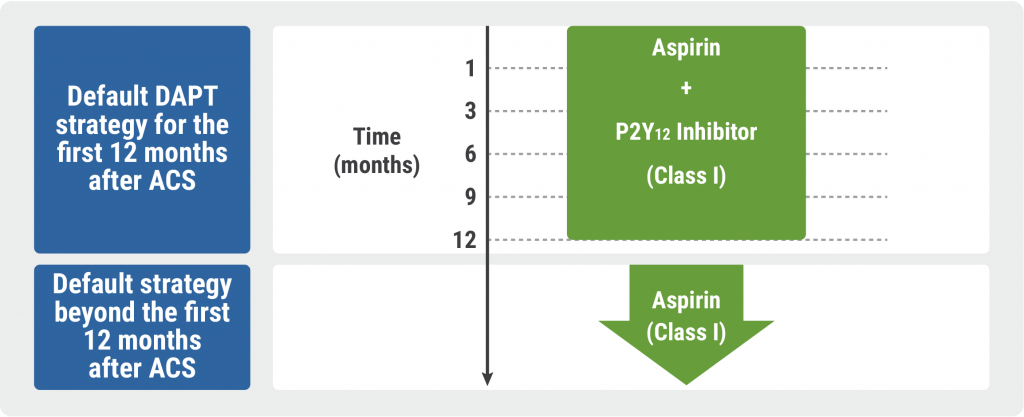
Guidelines for Acute Coronary Syndrome
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

