https://doi.org/10.55788/978444f2
“We know that patients with HIV have an increased risk of cardiovascular disease,” stated Dr Michael Lu (Massachusetts General Hospital, MA, USA) [1]. “Also, the moderate-intensity statin pitavastatin has minimal interaction with the antiretroviral therapy that is used by patients with HIV.” The phase 3 REPRIEVE trial (NCT02344290) randomised 7,769 participants with HIV on antiretroviral therapy with a low-to-moderate 10-year atherosclerotic cardiovascular disease (ASCVD) risk to pitavastatin calcium or placebo [2]. The primary analysis at 5.1 years showed a reduction of 35% in MACE in participants on pitavastatin compared with those who were treated with a placebo. The current analysis, presented by Dr Lu, evaluated the effect of pitavastatin on non-calcified coronary plaque formation and inflammatory and immune biomarkers in 804 participants.
At 24 months, the authors observed a reduction of 7% in non-calcified coronary plaque volume in participants on pitavastatin compared with those on placebo (95% CI -8.6 to -0.1; P=0.044). In participants with plaques at baseline, the corresponding difference was 12%. Furthermore, the risk of non-calcified plaque progression was 33% lower in the pitavastatin group than in the placebo group (95% CI 0.52–0.88; P=0.003).
“We also noted significant reductions in Lp-PLA2 and oxidised LDL levels in pitavastatin-treated individuals compared with placebo-treated individuals,” added Dr Lu. Changes in other biomarkers, such as MCP-1, sCD14, and IL-6, did not significantly differ between the 2 study groups at 24 months. “The results of REPRIEVE are in a similar ballpark with respect to plaque changes as other trials investigating LDL-reducing agents in higher-risk populations,” according to Dr Lu.
In conclusion, in a primary prevention population of patients with HIV and a low-to-moderate ASCVD risk, 2 years of pitavastatin treatment was associated with reduced non-calcified plaque volumes, a lower risk of plaque progression, and a reduction in relevant biomarkers of lipid oxidation and arterial inflammation, potentially explaining the reduction in MACE that was reported in the primary analysis of this trial.
- Lu MT, et al. Effects of pitavastatin on coronary artery disease and inflammatory biomarkers: mechanistic substudy of the REPRIEVE primary prevention trial in HIV. LB06, AHA Scientific Sessions 2023, 11–13 November, Philadelphia, USA.
- Grinspoon SK, et al. N Engl J Med 2023;389:687–699.
Copyright ©2024 Medicom Medical Publishers
Posted on
Previous Article
« Recaticimab may offer a solution for uncontrolled hypercholesterolaemia Next Article
Gene editing may change the treatment landscape of hypercholesterolaemia »
« Recaticimab may offer a solution for uncontrolled hypercholesterolaemia Next Article
Gene editing may change the treatment landscape of hypercholesterolaemia »
Table of Contents: AHA 2023
Featured articles
Abelacimab substantially lowers bleeding risk compared with rivaroxaban
Hot Topics in CAD/PAD
MINT: Liberal or restrictive transfusion strategy in MI with anaemia?
ORBITA-2 confirms PCI effective for symptom relief in patients with stable angina
Nicotinamide riboside shows promising trend for walking function in PAD
Pemafibrate reduces microvascular complications of PAD and T2D
Dapagliflozin improves cardiometabolic outcomes in myocardial infarction
Optimising Hypertension Outcomes
Edoxaban versus warfarin in chronic thromboembolic pulmonary hypertension
Sodium intake and blood pressure: new insights
Post-partum intervention lowers BP after hypertensive pregnancy
Biannual zilebesiran associated with substantial BP reductions
Future of Lipid-Lowering Therapies
Encouraging data for lepodisiran as Lp(a) lowering therapy
Gene editing may change the treatment landscape of hypercholesterolaemia
REPRIEVE: Mechanisms behind MACE reduction in HIV population on pitavastatin
Recaticimab may offer a solution for uncontrolled hypercholesterolaemia
Atrial Fibrillation and Sudden Cardiac Death
Abelacimab substantially lowers bleeding risk compared with rivaroxaban
Liraglutide may improve post-ablation outcomes in obese patients with AF
Single or dual cardioversion in patients with obesity and AF?
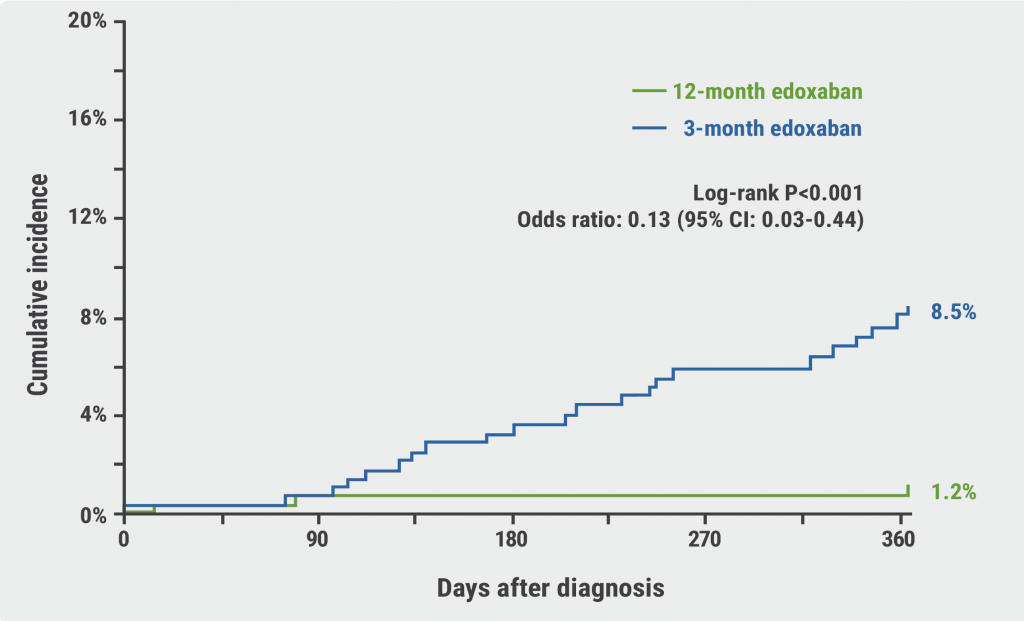
NOAH-AFNET 6: Does the duration of AHRE influence response to edoxaban?
ARTESIA: How useful is anticoagulation in subclinical AF?
Jewel IDE: High compliance rates for novel patch wearable cardioverter defibrillator
Sudden cardiac death in athletes: incidence, causes, and trends over 20 years
Miscellaneous Trials
Successful results for semaglutide in the highly anticipated SELECT trial
Can a walking intervention improve functional status and quality of life in HFrEF?
Head-to-head: Surgical embolectomy versus ultrasound-assisted thrombolysis in high-risk pulmonary embolism
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy