Prof. Naval Draver (University of Texas MD Anderson Cancer Centre, USA) presented the results of a phase 1b trial [1] examining the anti-CD47 antibody magrolimab in combination with azacitidine in patients with AML or high-risk MDS. The rationale of this study, he explained, is that CD47 is an immune checkpoint that lies on the surface of macrophages in AML. AML blast cells link CD47 to signal regulatory protein α. Because CD47 is a "do not eat me" signal, overexpression in AML leads to macrophage suppression and exhaustion, with consequent tumour evasion of phagocytosis by macrophages. Blocking CD47 with the first-in-class magrolimab, the investigators hypothesised, should lead to engulfment of leukaemic cells and reduction of tumour load. Moreover, preclinical data in immunodeficient mouse models have demonstrated prolonged survival and rapid responses with magrolimab in combination with the hypomethylating agent azacitidine [2]. Besides safety, co-primary endpoints were the objective response rate (ORR; response assessments according to 2006 IWG MDS criteria) and 8-week RBC transfusion-independence rate.
In total, 68 patients with either AML or high-risk MDS were treated with magrolimab in combination with azacitidine. The safety profile of the combination of magrolimab plus azacitidine was consistent with known effects of each agent individually, and no maximum tolerated dose was reached. Common all-grade treatment-related adverse events were anaemia (38%), fatigue (21%), neutropenia (19%), thrombocytopenia (18%), and infusion site reaction (16%). Only 1 patient discontinued the trial due to treatment-related adverse events.
The ORR primary endpoint was also met; of the 33 previously untreated high-risk MDS patients who were evaluable for efficacy, 91% achieved an objective response, including 42% with a complete remission (CR). Responses to magrolimab and azacitidine deepened over time, as the CR rate with >6 months of follow-up rose to 56%. In patients with previously untreated AML (n=25), 64% achieved an objective response, including 56% with a CR or a CR with incomplete blood count recovery (CRi). Notably, of the patients whose AML was characterised by a TP53-mutation (n=12), a particularly treatment-refractory and poor prognosis population, 75% achieved a CR or CRi. In total, 58% of RBC transfusion-dependent patients became transfusion-independent for at least 8 weeks. Median duration of response and median overall survival have not yet been reached. Follow-up and expansion cohorts are ongoing.
In short, magrolimab in combination with azacitidine is well-tolerated, and demonstrates robust activity in MDS and AML, including seemingly durable responses. Initial data indicate that this combination may be particularly effective but not exclusive against blast cells carrying TP53 mutation, a treatment-refractory subgroup. Registrational studies are being initiated.
- Draver N, et al. The first-in-class anti-CD47 antibody magrolimab combined with azacitidine is well-tolerated and effective in AML patients: phase 1b results. EHA25 Virtual, 11-21 June 2020, Abstract S144.
- Chao MP, et al. Therapeutic Targeting of the Macrophage Immune Checkpoint CD47 in Myeloid Malignancies. Front Oncol. 2020;9:1380.
Posted on
Previous Article
« Asciminib monotherapy in Ph+ CML: major molecular responses Next Article
DEC10-VEN superior to intensive chemotherapy in high-risk AML »
« Asciminib monotherapy in Ph+ CML: major molecular responses Next Article
DEC10-VEN superior to intensive chemotherapy in high-risk AML »
Table of Contents: EHA 2020
Featured articles
Myeloid
VIALE-A: newly diagnosed chemo-ineligible AML
DEC10-VEN superior to intensive chemotherapy in high-risk AML
Magrolimab plus azacitidine: good ORR in MDS/AML
Asciminib monotherapy in Ph+ CML: major molecular responses
CML TKI interruption: Swedish registry results
Patients with lower-risk MDS benefit from imetelstat
Better outcomes adding enasidenib to azacitidine in mIDH2-AML
Lymphoid
PET-stratification can omit radiotherapy in early-stage unfavourable Hodgkin lymphoma
Pembrolizumab improves PFS for relapsed/refractory Hodgkin lymphoma
Promising first-in-human trial of epcoritamab in B-NHL
Two trials: acalabrutinib in CLL
Zanubrutinib versus ibrutinib in Waldenström macroglobulinaemia
Deep responses in R/R CLL with venetoclax monotherapy
MRD assessment post-CAR-T predicts ALL allo-HSCT bridging
Plasma Cell Dyscrasias
Daratumumab for light-chain amyloidosis
Isatuximab triplet improves PFS in R/R MM
Initial results from CAR-T cell therapy in MM: KarMMa
Graft-Versus-Host Disease
GRAVITAS-301: improved complete aGVDH response
Ruxolitinib improves steroid-refractory aGVHD across subtypes
Benign Haematology
Paroxysmal nocturnal haemoglobinuria treatment with pegcetacoplan
Mitapivat, a pyruvate kinase-R activator, in SCD is safe with early efficacy results
SCD LentiGlobin gene therapy: new data on VOC and ACS
Paediatric Haematology
Venetoclax + navitoclax promising for R/R ALL or LL
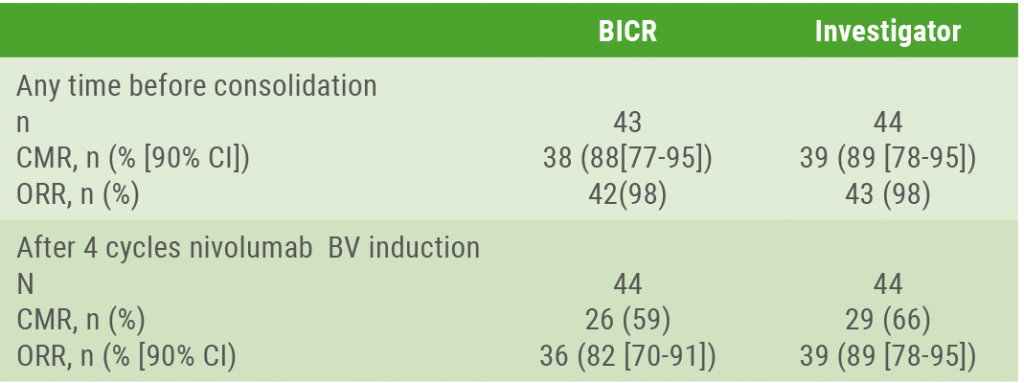
Nivolumab/brentuximab vedotin in R/R HL: good CMR rates
Bench-to-Bedside Science from the Presidential Symposium
Microbiome predicts B-ALL predisposition
Netrin-1 regulates haematopoietic stem cells
Unrecognised role of iron in neutrophil differentiation
Related Articles
August 28, 2020
Nivolumab/brentuximab vedotin in R/R HL: good CMR rates
September 9, 2020
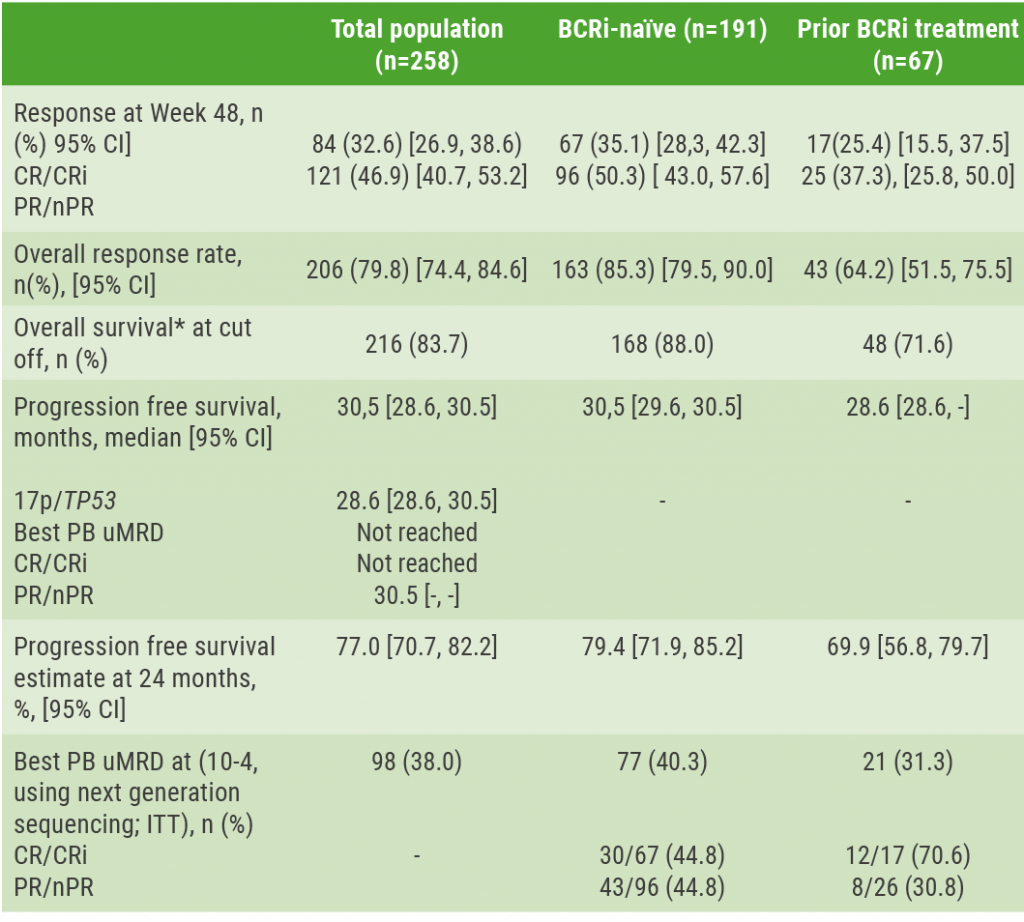
Deep responses in R/R CLL with venetoclax monotherapy
August 28, 2020
Endothelial damage in COVID-19
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

