Iron deficiency is a frequent comorbidity in heart failure with reduced ejection fraction (HFrEF), affecting approximately 50% of patients. Iron deficiency aggravates both functional status and clinical outcomes of patients with heart failure [1]. Progression of iron deficiency parallels an increased risk of worsening heart failure. FCM has been shown to reduce the risk for heart failure admission. Yet, the cardiac effects are relatively unknown. From a cardiac perspective, iron deficiency is associated with progressive cardiac remodelling, diminished cardiac/cardiomyocyte contractility, and reduced cardiac energy reserve. “The myocardium requires a lot of energy, for which you need iron,” Dr Pieter Martens (Hospital Oost-Limburg, Belgium) explained (see Figure) [2]. One of the operating mechanisms is the force-frequency relationship. In contrast to healthy controls, a reduced contractility is seen in HFrEF patients with increasing heart rate. “This energetic deficit worsens with iron deficiency,” Dr Martens added.
Figure: Iron deficiency and energy/contractility. Modified from [3,4]
 CK, creatine kinase; OXPHOS, oxidative phosphorylation; TCA, tricarboxylic acid cycle.
CK, creatine kinase; OXPHOS, oxidative phosphorylation; TCA, tricarboxylic acid cycle.
The rationale of the multicentre, randomised, double-blind, phase 4 IRON-CRT trial (NCT03380520) was to determine whether FCM induces incremental reverse remodelling in patients undergoing CRT with a persistently reduced LVEF and iron deficiency [2,5]. Moreover, the study assessed whether FCM could improve the force-frequency relationship in HFrEF. CRT patients were chosen specifically to perform a validated force-frequency pacing protocol.
The trial included adult patients with stable HFrEF and a CRT implant more than 6 months (n=75). All patients had a persistently reduced LVEF (<45%) and iron deficiency (ferritin <100 ng/mL or between 100-300 ng/mL if transferrin saturation was <20%). “Our patients were intensively treated: 50% of them received an angiotensin receptor neprilysin inhibitor on top of device therapy,” Dr Martens said. They were treated with either standard of care (n=37) or FCM (n=38). The primary endpoint was change in LVEF from baseline to 3 months. Change in left ventricular end-systolic volume (LVESV) and left ventricular end-diastolic volume (LVEDV) were assessed as secondary endpoints.
Significant improvement in primary and secondary endpoints
After 3 months, LVEF in the FCM group improved significantly compared with the standard-of-care group (P<0.001). LVEF increased in the FCM group by 4.22% (95% CI 3.05–5.38) compared with a decrease of 0.23% (95% CI -1.44 to 0.97) in the standard-of-care group. “We noticed an absolute improvement of about 4%,” Dr Martens said. The positive treatment effect of FCM was also noted in the secondary endpoints. LVESV was significantly decreased in the FCM group with 9.72 mL (95% CI -13.5 to -5.93) compared with a 1.83 mL decrease (95% CI -5.7 to 2.1) in the standard-of-care group (P=0.001). In addition, the force-frequency relationship changed from negative to positive. Therapy with FCM also improved maximal exercise capacity as measured by Peak VO2. A predefined subgroup analysis revealed that patients had a consistent beneficial treatment effect independent of their LVEF, haemoglobin, or transferrin saturation at baseline.
“We did not observe more adverse events in the FCM groups compared with placebo,” Dr Martens said. Therefore, he concluded that therapy with FCM in HF patients with persistently reduced LVEF despite optimal medical therapy and CRT over 3 months resulted in cardiac reverse remodelling (documented by a change in LVEF and LVESV) and an improvement in cardiac performance. Thus, the IRON-CRT trial further expands knowledge on the mode-of-action of FCM in HFrEF.
- Martens P, et al. Acta Cardiol 2018:73(2):115-23.
- Martens P, et al. The effect of intravenous ferric-carboxymaltose on cardiac reverse remodeling following cardiac resynchronization therapy – The IRON CRT trial. LBT 1, Heart Failure and World Congress on Acute Heart Failure 2021, 29 June–1 July.
- Martens P, et al. Eur J Heart Fail 2018;20(5):920-2.
- Martens P, et al. Eur J Heart Fail 2018;20(4):806-8.
- Martens P, et al. Eur. Heart J. 2021. DOI: 1093/eurheartj/ehab411.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Novel mineralocorticoid receptor antagonist effective irrespective of HF history Next Article
Electronic nose could track action of anti-PD-1 therapy in lung cancer »
« Novel mineralocorticoid receptor antagonist effective irrespective of HF history Next Article
Electronic nose could track action of anti-PD-1 therapy in lung cancer »
Table of Contents: HFA 2021
Featured articles
Inconclusive results for dapagliflozin treatment in heart failure
Late-Breaking Trials
Iron substitution improves LVEF in intensively treated CRT patients with iron deficiency
Novel mineralocorticoid receptor antagonist effective irrespective of HF history
Iron substitution in iron-deficient HF patients is highly cost-effective
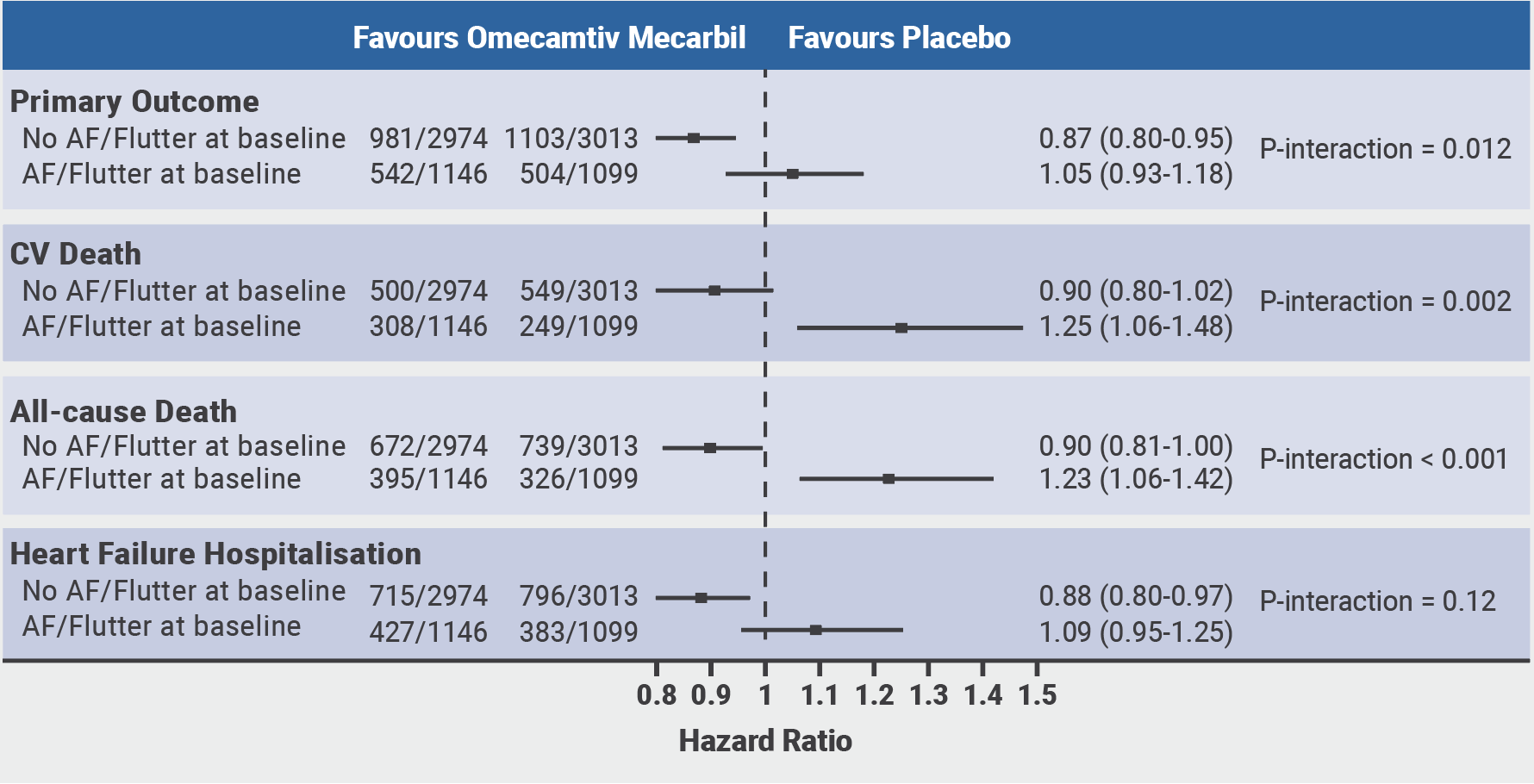
Omecamtiv mecarbil might be less effective in patients with atrial fibrillation or flutter
Vericiguat effective irrespective of atrial fibrillation status
Baroreflex activation: a novel option to improve heart failure symptoms
Beta-blocker withdrawal to enhance exercise capacity in heart failure?
Inconclusive results for dapagliflozin treatment in heart failure
Computerised cognitive training improves cognitive function in HF patients
COVID-19 and the Heart
COVID-19-related HF: from systemic infection to cardiac inflammation
Myocardial infarction outcomes were significantly affected by the pandemic
TAPSE effective biomarker associated with high-risk of severe COVID-19
COVID-19 in AF patients with HF: no higher mortality but longer hospital stay
Cancer and the Heart
Heart failure patients might be at an increased risk for head and neck cancer
Trastuzumab associated with cardiotoxicity in breast cancer
Heart Failure Prevention and HRQoL in the 21st century
Psychoactive substances put young people at risk of cardiovascular disease
The challenge of improving the quality of life of heart failure patients
SGLT2 Inhibitors in Heart Failure
Empagliflozin linked to lower cardiovascular risk and renal events in real-world study
Efficacy of dapagliflozin and empagliflozin not influenced by diabetes status
Biomarker panel predicts SGLT2 inhibitor response
Best of the Posters
Real-world study suggests sacubitril/valsartan benefits elderly patients with HF
Proenkephalin: A useful biomarker for new-onset heart failure?
Weight loss associated with increased mortality risk in heart failure patients
Echocardiographic parameters linked to dementia diagnosis
Related Articles

July 20, 2021
HFA 2021 Highlights Podcast
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

