As there is a high prevalence of concomitant heart failure (HF) in diabetics, the impact of anti-diabetic medication on cardiovascular and renal outcomes may play a role in HF therapy [1]. A large, non-interventional study compared type 2 diabetes treatment with the sodium-glucose cotransporter-2 (SGLT2) inhibitor empagliflozin with therapy with a DPP-4 inhibitor in terms of primary cardiovascular and secondary renal effectiveness outcomes [2].
Between 2014 and 2019, data was collected from large databases and registries in Sweden, Finland, Germany, Spain, and Isreal. Included were >75,000 adults who started diabetes treatment with either empagliflozin (n=38,203) or a DPP-4 inhibitor (n=38,203). The mean age was a little over 60 years, and most patients were men. Logistic regression was used for the analysis based on propensity score matching.
Prof. Leo Niskanen (University of Eastern Finland, Finland) presented the results as pooled incidence rates and hazard ratios for the comparison of empagliflozin versus DPP-4 inhibitor. The incidence rate of hospitalisation for HF was 7.36 per 1,000 patient-years with empagliflozin compared with 11.86 per 1,000 patient-years with DPP-4 inhibitor (HR 0.60; 95% CI 0.50–0.72; see Table). Likewise, an HR of 0.52 (95% CI 0.39–0.69) for all-cause mortality indicated significant superiority of empagliflozin. “If we then look at the composite outcome including hospitalisation for HF and all-cause mortality, we can see that this was clearly in favour of empagliflozin with a 40% lower risk, which was highly significant,” Prof. Niskanen pointed out.
Table: Empagliflozin versus DPP-4 inhibitor reduced the risk of cardiovascular and renal events in the EMPRISE study [2] Shown are pooled incidence rates and pooled hazard ratios of events among empagliflozin versus DPP-4 inhibitor users in 1:1 propensity score-matched populations.
Shown are pooled incidence rates and pooled hazard ratios of events among empagliflozin versus DPP-4 inhibitor users in 1:1 propensity score-matched populations.
CI, confidence interval; DDP-4i, dipeptidyl peptidase-4 inhibitor; EMPA, empagliflozin; FU, follow-up; HR, hazard ratio; IR, incidence rate; MI, myocardial infarction; PY, patient-years.
The second composite of myocardial infarction, stroke, and all-cause mortality, resulted in a 36% reduced likelihood for patients in the empagliflozin group (HR 0.64; 95% CI 0.52–0.80). The researchers also assessed myocardial infarction, stroke (pooled HR 0.71; 95% CI 0.56–0.90), and end-stage renal disease (pooled HR 0.40; 95% CI 0.17–0.95) for empagliflozin versus DPP-4 inhibitor. However, the individual outcome of myocardial infarction was non-significant (HR 0.95; 95% CI 0.74–1.22).
“These results complement the results from the clinical trial EMPA-REG OUTCOME (NCT01131676) and support changes recently made in the ADA and EASD consensus update,” underlined Prof. Niskanen in his conclusion.
- Lehrke M, et al. Am J Cardiol. 2017;120(1S):S37–S47.
- Niskanen L, et al. Empagliflozin use versus dipeptidyl peptidase 4 inhibitors reduces risk of cardiovascular. Heart Failure and World Congress on Acute Heart Failure 2021, 29 June–1 July.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Efficacy of dapagliflozin and empagliflozin not influenced by diabetes status Next Article
Myocardial infarction outcomes were significantly affected by the pandemic »
« Efficacy of dapagliflozin and empagliflozin not influenced by diabetes status Next Article
Myocardial infarction outcomes were significantly affected by the pandemic »
Table of Contents: HFA 2021
Featured articles
Inconclusive results for dapagliflozin treatment in heart failure
Late-Breaking Trials
Iron substitution improves LVEF in intensively treated CRT patients with iron deficiency
Novel mineralocorticoid receptor antagonist effective irrespective of HF history
Iron substitution in iron-deficient HF patients is highly cost-effective
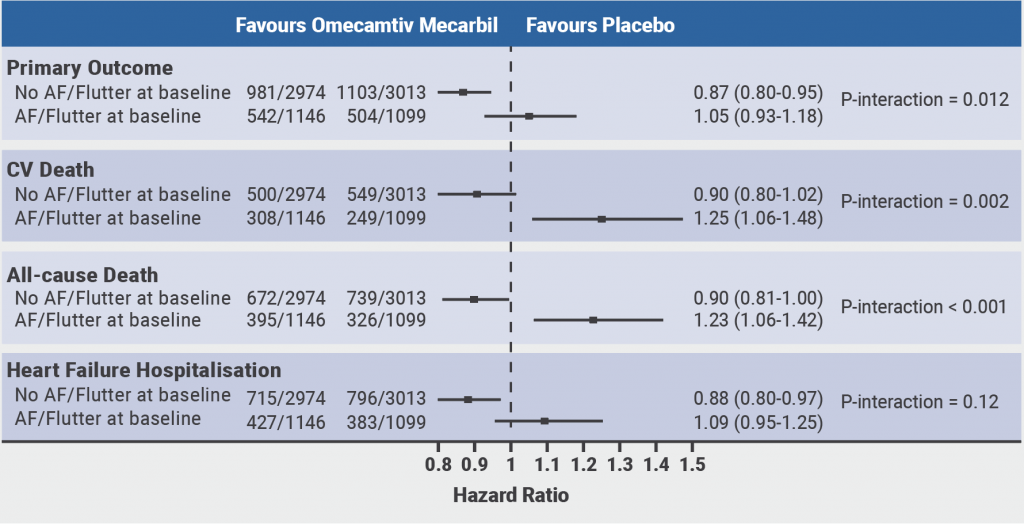
Omecamtiv mecarbil might be less effective in patients with atrial fibrillation or flutter
Vericiguat effective irrespective of atrial fibrillation status
Baroreflex activation: a novel option to improve heart failure symptoms
Beta-blocker withdrawal to enhance exercise capacity in heart failure?
Inconclusive results for dapagliflozin treatment in heart failure
Computerised cognitive training improves cognitive function in HF patients
COVID-19 and the Heart
COVID-19-related HF: from systemic infection to cardiac inflammation
Myocardial infarction outcomes were significantly affected by the pandemic
TAPSE effective biomarker associated with high-risk of severe COVID-19
COVID-19 in AF patients with HF: no higher mortality but longer hospital stay
Cancer and the Heart
Heart failure patients might be at an increased risk for head and neck cancer
Trastuzumab associated with cardiotoxicity in breast cancer
Heart Failure Prevention and HRQoL in the 21st century
Psychoactive substances put young people at risk of cardiovascular disease
The challenge of improving the quality of life of heart failure patients
SGLT2 Inhibitors in Heart Failure
Empagliflozin linked to lower cardiovascular risk and renal events in real-world study
Efficacy of dapagliflozin and empagliflozin not influenced by diabetes status
Biomarker panel predicts SGLT2 inhibitor response
Best of the Posters
Real-world study suggests sacubitril/valsartan benefits elderly patients with HF
Proenkephalin: A useful biomarker for new-onset heart failure?
Weight loss associated with increased mortality risk in heart failure patients
Echocardiographic parameters linked to dementia diagnosis
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy