“In patients with HFrEF, SGLT2 inhibitors have been shown to improve symptoms, to reduce HF hospitalisations, and even to improve survival, but we don’t know their effect on walking distance,” said Prof. John McMurray (University of Glasgow, UK) [1]. Prof. McMurray presented the results of the DETERMINE trials, which investigated the effect of dapagliflozin on symptoms and exercise capacity in HF patients.
DETERMINE-Reduced (D-R; NCT03877237) enrolled 313 patients with HFrEF and DETERMINE-Preserved (D-P; NCT03877237) 504 patients with HFpEF. All patients had to be on stable treatment, demonstrated an initial performance of ≥100 metres and ≤425 metres in 6-minute walking distance (6MWD) testing, and also had an estimated glomerular filtration rate of ≥25 mL/min/1.73m2. The participants differed in left ventricular ejection fraction (≤40% in D-R and >40% in D-P) and the trials used different inclusion cut-offs for N-terminal pro B-type natriuretic peptide (NT-proBNP; ≥400 pg/mL in D-R and ≥250 pg/mL in D-P). In both trials, patients were randomised 1:1 to receive a daily dose of 10 mg dapagliflozin or placebo over 16 weeks. The primary endpoint consisted of 3 components: reduction in patient-reported HF symptoms, reduction in patient-reported physical limitations, and improvement of walking distance.
In D-R, the baseline characteristics in the dapagliflozin and the placebo arm were balanced. The mean age was 68.4 and 67.3 years, 71.2% and 77.7% were men, and 83.3% and 79.6% were in NYHA class II, respectively. Baseline Kansas City Cardiomyopathy Questionnaire (KCCQ)-total symptom scores (TSS) were 79.2 in the dapagliflozin versus 80.2 in the placebo arm with correspondent values of 70.8 versus 75.0 in the KCCQ-physical limitation score (PLS) and 327.5 versus 344.0 metres in 6MWD. The results showed an average significant mean difference of 4.23 points in TSS (P=0.022) between dapagliflozin and placebo. Also, more patients reported a moderate or large improvement of ≥15 points in TSS, translating into a significant odds ratio (OR) of 1.6 (95% CI 1.0–2.7). The results in PLS (OR 1.6; 95% CI 0.9–2.6) and 6MWD (OR 1.1; 95% CI 0.7–1.8) failed to demonstrate a significant disparity between the study groups.
In the D-P trial, the overall mean patient age was 72 years, 63.5% were men, over 40% suffered from type 2 diabetes, and over 80% were NYHA class II. Median scores for TSS were between 77.1 and 78.1 and for PLS between 70.8 and 75.0. Median 6MWD was 320 metres. Interestingly, the assessment of possible treatment effects revealed no significantly different results in TSS, PLS, and 6MWD in the dapagliflozin versus the placebo arm.
Of note, the evaluation of exploratory outcomes in both trials showed a clear reduction in NT-proBNP with nominal P-values of 0.013 in D-R and 0.024 in D-P in favour of dapagliflozin therapy.
“At the moment, the therapeutic role of SGLT inhibition in HEpEF remains uncertain, although we are going to hear the results of a large trial in the next few weeks,” Prof. McMurray added.
- McMurray JJV. Effect of dapagliflozin vs placebo on symptoms and six-minute walk distance in patients with heart failure. LBT 3, Heart Failure and World Congress on Acute Heart Failure 2021, 29 June–1 July.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
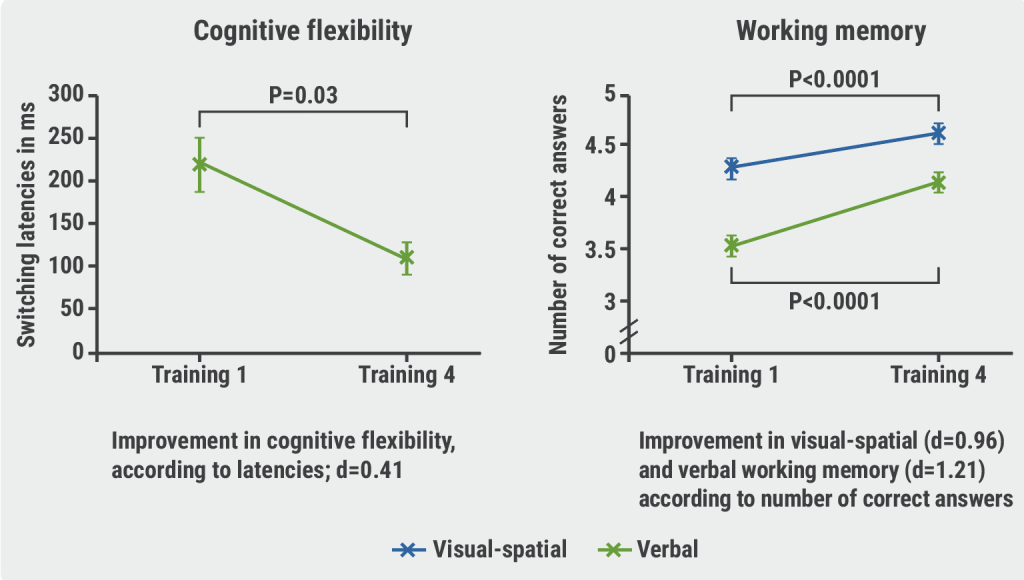
« Computerised cognitive training improves cognitive function in HF patients Next Article
Beta-blocker withdrawal to enhance exercise capacity in heart failure? »
« Computerised cognitive training improves cognitive function in HF patients Next Article
Beta-blocker withdrawal to enhance exercise capacity in heart failure? »
Table of Contents: HFA 2021
Featured articles
Inconclusive results for dapagliflozin treatment in heart failure
Late-Breaking Trials
Iron substitution improves LVEF in intensively treated CRT patients with iron deficiency
Novel mineralocorticoid receptor antagonist effective irrespective of HF history
Iron substitution in iron-deficient HF patients is highly cost-effective
Omecamtiv mecarbil might be less effective in patients with atrial fibrillation or flutter
Vericiguat effective irrespective of atrial fibrillation status
Baroreflex activation: a novel option to improve heart failure symptoms
Beta-blocker withdrawal to enhance exercise capacity in heart failure?
Inconclusive results for dapagliflozin treatment in heart failure
Computerised cognitive training improves cognitive function in HF patients
COVID-19 and the Heart
COVID-19-related HF: from systemic infection to cardiac inflammation
Myocardial infarction outcomes were significantly affected by the pandemic
TAPSE effective biomarker associated with high-risk of severe COVID-19
COVID-19 in AF patients with HF: no higher mortality but longer hospital stay
Cancer and the Heart
Heart failure patients might be at an increased risk for head and neck cancer
Trastuzumab associated with cardiotoxicity in breast cancer
Heart Failure Prevention and HRQoL in the 21st century
Psychoactive substances put young people at risk of cardiovascular disease
The challenge of improving the quality of life of heart failure patients
SGLT2 Inhibitors in Heart Failure
Empagliflozin linked to lower cardiovascular risk and renal events in real-world study
Efficacy of dapagliflozin and empagliflozin not influenced by diabetes status
Biomarker panel predicts SGLT2 inhibitor response
Best of the Posters
Real-world study suggests sacubitril/valsartan benefits elderly patients with HF
Proenkephalin: A useful biomarker for new-onset heart failure?
Weight loss associated with increased mortality risk in heart failure patients
Echocardiographic parameters linked to dementia diagnosis
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy