Dr Courtney Di Nardo (MD Anderson Cancer Centre, USA) presented the results. Enasidenib is a small-molecule inhibitor of the mutant IDH2 protein, present in a subset of AMLs, and it has been hypothesised that it might be synergistic with azacitidine.
A total of 101 patients (median age, 75 years) were enrolled and randomised to combination therapy (n=68) or azacitidine monotherapy (n=33). All patients received azacitidine subcutaneously at 75 mg/m2 for 7 days of each 28-day cycle. Patients in the combination therapy arm received oral enasidenib at 100 mg once daily throughout the study. The median number of treatment cycles was 10 (range 1-26) in the combination therapy arm and 6 (range 1-28) in the azacitidine monotherapy arm. A total of 7 patients in the azacitidine monotherapy arm crossed-over to receive subsequent treatment with enasidenib. The primary endpoint of this portion of the trial was overall response rate (ORR). Key secondary endpoints included duration of response (DOR), overall survival (OS), and event-free survival (EFS).
The primary endpoint was met; ORR was 48% in the combination therapy arm compared with 14% with azacitidine monotherapy. However, the secondary endpoint of median OS was not met; both of the treatment arms had a median OS of 22 months (HR 0.99; 95% CI 0.52-1.87; P=0.97), which may be attributable to the fact that most patients from the azacitidine monotherapy arm received enasidinib after they left the study. Despite a numerical difference, median EFS was also not met: 17.2 months in the combination arm versus 10.8 months for azacitidine monotherapy (HR 0.59; 95% CI 0.30-1.17; P=0.13).
The most common treatment-related grade 3-4 adverse events (AEs) with enasidenib plus azacitidine were thrombocytopenia (37% vs 19% with azacitidine monotherapy), neutropenia (35% vs 22%, respectively), anaemia (19% vs 22%, respectively), and febrile neutropenia (15% vs 16%, respectively). Grade 3-4 infections were reported in 18% and 31% of patients in each arm, respectively. The most common reason for treatment discontinuation was disease progression.
- DiNardo C, et al. Enasidenib plus azacitidine significantly improves complete remission and overall response rates versus azacitidine monotherapy in mutant-IDH2 newly diagnosed acute myeloid leukemia (ND-AML). EHA25 Virtual, 11-21 June 2020, Abstract S139.
Posted on
Previous Article
« PET-stratification can omit radiotherapy in early-stage unfavourable Hodgkin lymphoma Next Article
Patients with lower-risk MDS benefit from imetelstat »
« PET-stratification can omit radiotherapy in early-stage unfavourable Hodgkin lymphoma Next Article
Patients with lower-risk MDS benefit from imetelstat »
Table of Contents: EHA 2020
Featured articles
Myeloid
VIALE-A: newly diagnosed chemo-ineligible AML
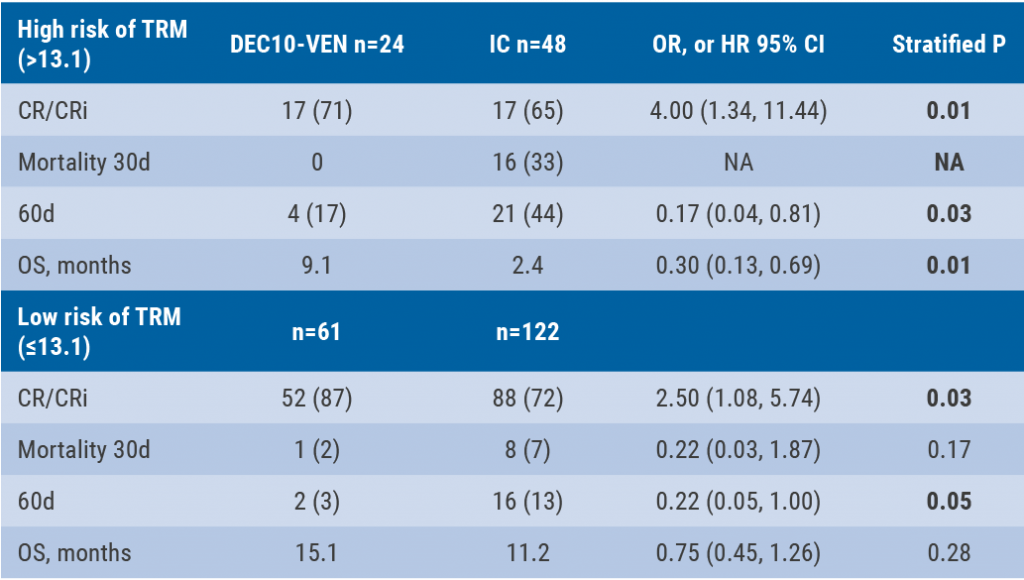
DEC10-VEN superior to intensive chemotherapy in high-risk AML
Magrolimab plus azacitidine: good ORR in MDS/AML
Asciminib monotherapy in Ph+ CML: major molecular responses
CML TKI interruption: Swedish registry results
Patients with lower-risk MDS benefit from imetelstat
Better outcomes adding enasidenib to azacitidine in mIDH2-AML
Lymphoid
PET-stratification can omit radiotherapy in early-stage unfavourable Hodgkin lymphoma
Pembrolizumab improves PFS for relapsed/refractory Hodgkin lymphoma
Promising first-in-human trial of epcoritamab in B-NHL
Two trials: acalabrutinib in CLL
Zanubrutinib versus ibrutinib in Waldenström macroglobulinaemia
Deep responses in R/R CLL with venetoclax monotherapy
MRD assessment post-CAR-T predicts ALL allo-HSCT bridging
Plasma Cell Dyscrasias
Daratumumab for light-chain amyloidosis
Isatuximab triplet improves PFS in R/R MM
Initial results from CAR-T cell therapy in MM: KarMMa
Graft-Versus-Host Disease
GRAVITAS-301: improved complete aGVDH response
Ruxolitinib improves steroid-refractory aGVHD across subtypes
Benign Haematology
Paroxysmal nocturnal haemoglobinuria treatment with pegcetacoplan
Mitapivat, a pyruvate kinase-R activator, in SCD is safe with early efficacy results
SCD LentiGlobin gene therapy: new data on VOC and ACS
Paediatric Haematology
Venetoclax + navitoclax promising for R/R ALL or LL
Nivolumab/brentuximab vedotin in R/R HL: good CMR rates
Bench-to-Bedside Science from the Presidential Symposium
Microbiome predicts B-ALL predisposition
Netrin-1 regulates haematopoietic stem cells
Unrecognised role of iron in neutrophil differentiation
Related Articles
September 9, 2020
DEC10-VEN superior to intensive chemotherapy in high-risk AML
September 9, 2020
Zanubrutinib versus ibrutinib in Waldenström macroglobulinaemia
September 9, 2020
CML TKI interruption: Swedish registry results
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

