TNFi therapy is effective in controlling several rheumatic diseases and more specifically has been shown to reduce pain. NSAIDs are commonly used for the management and treatment of pain and stiffness in inflammatory arthritides and are the first-line treatment for axial spondyloarthritis. Dr Olafur Palsson (University Hospital Reykjavik, Iceland) et al. aimed to gain a better understanding of the consumption of NSAIDs in patients with rheumatoid arthritis (RA), psoriatic arthritis (PsA), and ankylosing spondylitis (AS) as compared with the general population, as well as to explore their relationship with disease activity measures. Additionally, the impact of TNFi therapy on NSAID prescription rates was evaluated.
To accomplish these goals, the research group initiated ICEBIO, an Icelandic nationwide database on patients treated with biological disease-modfiying anti-rheumatic drugs (DMARDs) due to inflammatory joint diseases; including RA, PsA, and AS. Data for all patients with inflammatory arthritis was extracted along with all filed prescriptions for NSAIDs made 2 years before and 2 years after the initiation of TNFi therapy. This is available through the Icelandic Directorate of Health, which operates a prescription database that includes over 90% of all drug prescriptions in Iceland. For each patient, NSAID prescriptions of 5 randomly selected individuals matched on age, sex, and calendar time of TNF inhibition were extracted as a control. As such, data of 952 patients was included (366 RA, 251 PsA, 218 AS) along with 4,760 controls. The drug database yielded a total of 5,600 and 8,600 prescriptions for patients and controls, respectively.
The control group was prescribed a mean of 23 defined daily doses (DDD) of NSAIDs per year. In total, the ICEBIO patients were prescribed 6.7 times more DDDs of NSAIDs than the controls at a mean of 149 per year. After initiation of TNFi therapy, the use of NSAIDs was reduced to a mean of 85 DDD per year, or 3.9 times that of the controls. Consumption was reduced by 43% (mean 148 to 85 DDD/year) in RA patients, 43% in the PsA group (157 to 90 DDD/year), and 47% in the AS group (154 to 83 DDD/year).
In terms of measuring disease activity, the group was divided into the 20% of patients who consumed the highest amount of NSAIDs and the remaining 80%. These groups were very similar in patient demographics, although the high-consuming patient group trended towards longer disease. When TNFi therapy was initiated, the 2 groups appeared to be similarly related with regard to number of swollen (4.5 to 4.2) or tender (5.4 to 5.5) joints in RA, or to physician global VAS assessment (56 vs 57). On the other hand, patient-reported outcome measures revealed small but significant differences between groups. The high-consuming patient group reported worse VAS pain scores (65 vs 60), VAS global health scores (70 vs 65), and HAQ-DI scores (1.19 vs 1.03).
- Palsson O, et al. Abstract OP0001. EULAR 2019.
Posted on
Previous Article
« Switch to sarilumab from adalimumab is efficacious and safe Next Article
Unacceptable pain is common in patients with psoriatic arthritis »
« Switch to sarilumab from adalimumab is efficacious and safe Next Article
Unacceptable pain is common in patients with psoriatic arthritis »
Table of Contents: EULAR 2019
Featured articles
Efficacy and safety of ixekizumab versus adalimumab in patients with PsA
Rheumatoid Arthritis
Cohort study shows improvement during 25 years of RA treatment
Filgotinib in RA patients with inadequate response or naïve to methotrexate
Clinical effectiveness of fenebrutinib in RA patients with methotrexate or TNFi failure
Short methotrexate stop is safe in patients with RA
Tofacitinib is safe according to real-world data analysis
Tapering of prednisone in RA patients who achieved low disease activity or remission with tocilizumab
Efficacy and safety of E6011 in RA patients with inadequate response to methotrexate
Preliminary efficacy and safety data of RG6125 in RA patients with an inadequate response to TNF inhibitors
Integrated 10-year analysis confirms safety profile abatacept
Switching among multiple infliximab biosimilars does not cause immunogenicity
Switch to sarilumab from adalimumab is efficacious and safe
Axial Spondyloarthritis
Treat-to-target approach emerging in axial spondyloarthritis
NSAIDs consumption is linked to patient-assessed disease activity and decreases with use of TNF inhibitors
Psoriatic Arthritis
Efficacy and safety of ixekizumab versus adalimumab in patients with PsA
Efficacy and safety of bimekizumab in patients with active PsA
Filgotinib is efficacious and safe in PsA
Ixekizumab improves signs and symptoms in TNFi-naïve PsA patients
Etanercept and methotrexate as first-line treatment in PsA
Unacceptable pain is common in patients with psoriatic arthritis
Osteoarthritis and Osteoporosis
Miscellaneous
Interstitial lung disease in rheumatic diseases and systemic sclerosis
Emapalumab in patients with macrophage activation syndrome
Support for tocilizumab use in giant cell arteritis
Related Articles

September 4, 2019
Letter from the Editor
September 4, 2019
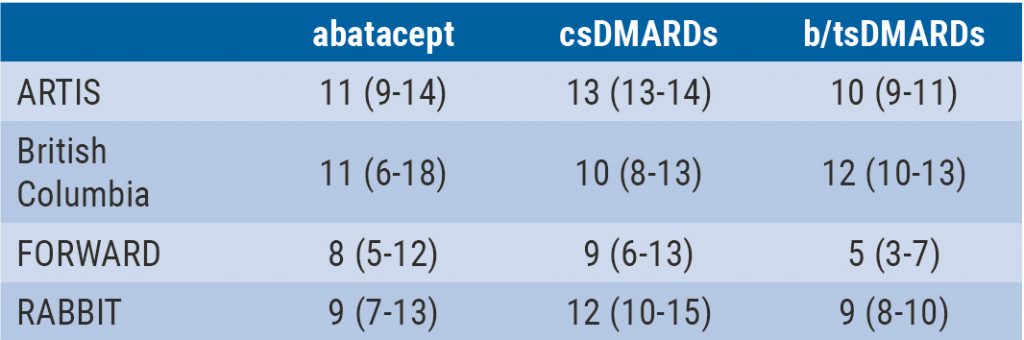
Integrated 10-year analysis confirms safety profile abatacept
September 4, 2019
Efficacy and safety of bimekizumab in patients with active PsA
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

