Dr Shah and colleagues hypothesised that ischaemic preconditioning of the myocardium may have a protective effect in some sleep apnoea (SA) patients during myocardial infarction (MI). The researchers conducted a study to assess whether sleep apnoea is associated with reduced infarct size and enhanced coronary collaterals during an MI by quantifying infarct size (% of left ventricle [LV] infarcted divided by the volume of LV mass). They assessed the score of coronary collaterals using the Rentrop Score (range 0-3, higher scores indicating augmented collaterals).
The study recruited 33 patients (age >21) with ST-elevation MI who underwent percutaneous coronary intervention. Level 3 SA testing was done during hospitalisation. Patients were stratified by SA severity: none (apnoea-hypopnoea index [AHI]<5, n=8), mild (5≤AHI<15, n=10), moderate (15≤AHI<30, n=8), and severe (AHI>30, n=7) (hypopneas with 4% desaturation). Comparing the no-SA vs SA groups, the mean age was 47.5±10.9 years vs 56.6±11.0 years, mean BMI (kg/m2) 26.4±6.11) vs 29.3±5.82, male gender 87.5% vs 88%. The median infarct size in no-SA was 22% vs 28% in the SA group (P=0.79). Across all SA categories, moderate SA group had the lowest infarct size (median 15.5; IQR 9-23) vs mild SA (median 27, IQR 23.8-32.5) and severe SA (median 34, IQR 31-53, P=0.289). Similarly, moderate SA group had the highest Rentrop grade compared with no-SA, mild SA, or severe SA (P=0.23). After excluding central SA, moderate SA patients had a significantly higher proportion of Rentrop grade 2 (indicating higher collaterals) compared with other SA categories (P=0.03).
The study results generate preliminary evidence for a non-linear relationship between SA severity and infarct size where only moderate SA appears to be associated with reduced infarct size and enhanced coronary collaterals. Dr Shah noted that these data were consistent with animal models of hypoxic preconditioning. The study suggests that moderate SA may be cardioprotective in acute MI through enhanced collaterals, but this requires confirmation in larger studies adjusted for intergroup differences.
In an interview, Dr Shah added, “I think that sleep apnoea for the last 2 decades has been a well-established independent risk factor for cardiovascular disease, and we have done many, many studies that have shown that sleep apnoea is an independent risk factor for stroke, for arrhythmias, for sudden cardiac death, for atrial fibrillation, for myocardial infarction. But unfortunately, in the recent few years, the clinical trials in which we are trying to treat the sleep apnoea condition with continuous positive airway pressure, therapy did not reduce the occurrence of some of these events. So, it is a little puzzling, because we have shown that it is a risk factor for cardiovascular disease, but when we treated, it did not really make the impact that we were hoping for it to make. We are in a state of a little bit of confusion, and we are really trying to dig deep in terms of the mechanisms—as to what it is about the obstructive sleep apnoea that was causing this increased risk factor.”
- Shah NA. A4460, ATS 2019, 17-22 May, Dallas, USA.
Posted on
Previous Article
« Pulmonary arterial hypertension: early treatment with selexipag most effective Next Article
CRISPR/Cas9 genome editing therapy of hereditary pulmonary alveolar proteinosis »
« Pulmonary arterial hypertension: early treatment with selexipag most effective Next Article
CRISPR/Cas9 genome editing therapy of hereditary pulmonary alveolar proteinosis »
Table of Contents: ATS 2019
Featured articles
Letter from the Editor
Interview with Prof. Christian Bergmann
Treatable Traits in Chronic Inflammatory Airway Disease: Back to Basics
Treatable traits in chronic inflammatory airway disease: back to basics
Critical Care Medicine
Distinguishing between 4 different subtypes of sepsis sets the stage for individualised treatment
Stem cell therapy in acute respiratory distress syndrome improves 28-day mortality
SPICE III trial: Early sedation with dexmedetomidine in critically ill patients
SAATELLITE trial: Suvratoxumab prevents ventilator-associated Staphylococcus Aureus pneumonia in intensive care unit patients
Sleep Medicine
Million-patient study reveals gaps in long-term adherence among various sub-populations
Sleep apnoea severity has a non-linear relationship with acute myocardial infarction risk
Obstructive sleep apnoea affects morning spatial navigational memory processing in asymptomatic older individuals
Pulmonary Vascular Disease and Interstitial Lung Disease
Nintedanib reduces lung function decline in systemic sclerosis-associated ILD
Pulmonary arterial hypertension: early treatment with selexipag most effective
Long-term safety and efficacy of recombinant human pentraxin-2 in patients with idiopathic pulmonary fibrosis
Infection
Dupilumab improves outcomes in patients with severe chronic rhinosinusitis with nasal polyps and comorbid asthma
Durability of culture conversion in patients receiving ALIS for treatment-refractory MAC lung disease
E-cigarette use disrupts normal immune response to viral infections, particularly in women
Paediatric Pulmonary Medicine
Bacterial pneumonia predicts ongoing lung problems in infants hospitalised for acute respiratory failure
Aspergillus and early cystic fibrosis lung disease: does it need to be treated?
COPD
CORTICO-COP trial: eosinophil-guided therapy reduces systemic corticosteroid exposure
A randomised controlled trial of a smoking cessation smartphone application
Benralizumab does not ameliorate COPD exacerbations (GALATHEA/TERRANOVA trials)
Aclidinium bromide delays COPD exacerbation without increased MACE risk
Bench-to-Bedside (Pre-Clinical)
Human lung organoids to study foetal RSV infection
CRISPR/Cas9 genome editing therapy of hereditary pulmonary alveolar proteinosis
Cilia diagnostics in primary ciliary dyskinesia
Tuberous sclerosis complex 2 may be a novel target in pulmonary arterial hypertension therapy
Related Articles
November 7, 2018
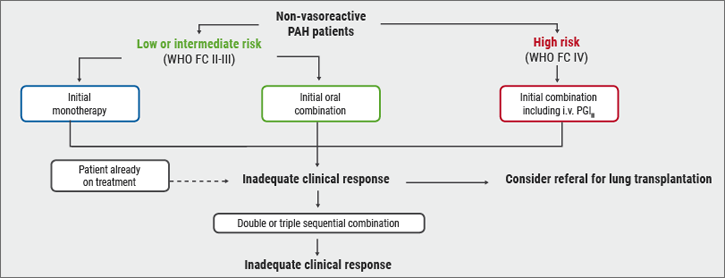
Risk stratification
August 18, 2021
Hypertension pathology visible in white matter lesion volume
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

