Hereditary pulmonary alveolar proteinosis (hPAP) is a rare disease characterised by surfactant accumulation in pulmonary alveoli resulting in respiratory failure. The disease is caused by mutations in the granulocyte-macrophage colony-stimulating factor (GM-CSF) receptor alpha or beta subunit genes (CSF2RA or CSF2RB) resulting in impaired GM-CSF-dependent surfactant clearance by alveolar macrophages. Typical CT and histological hallmarks of the disease are used for diagnosis. Dr Shima’s team has previously generated human induced pluripotent stem cells (iPSCs) from hPAP patients [2]. iPSCs are derived from the somatic cells (in this case, fibroblasts from a skin biopsy) and reprogrammed back into a pluripotent state. The pluripotent iPSCs can then be differentiated to a wide range of tissues and cell types. iPSCs can be used for in vitro disease modelling, in vitro drug screening, and patient-specific cell therapy investigations. In rare diseases like hPAP, it can be difficult to acquire patient samples, thus iPSC cells are a useful tool to investigate pathogenesis. Dr Shima and colleagues characterised iPSC-derived macrophages that retained disease-specific features in functional tests of GM-CSF signalling. The authors had previously demonstrated that lentiviral vector-mediated reconstitution of CSF2RA restored GM-CSF signalling and function in hPAP iPSC-derived macrophages derived from a patient with CSF2RA mutations [2]. The team hypothesised that CRISPR/Cas9 genome editing could repair the impaired function of hPAP-iPSC-derived macrophages and overcome the limitations of viral vector-mediated gene therapy such as insertional mutagenesis and pose a better potential therapy for patients.
The researchers generated wild-type CSF2RA guide-RNA for CRISPR/Cas9 genome editing aimed at correcting the truncating mutation CSF2RAR217X (CSF2RAc.649C>T gene mutation). The double stranded break generated by CRISPR/Cas9 was repaired by homology-directed repair using the provided wild-type guide RNA, to correct the gene mutation in situ.
The investigators then terminally differentiated the “corrected” patient fibroblasts to macrophages, in two steps: first by using a kit to differentiate to haematopoietic stem cells, and then to further differentiate to macrophages by culturing in the presence of GM-CSF and macrophage colony-stimulating factor, and performed functional analyses compared with the original (isogenic) patient fibroblasts. Firstly, macrophage surface markers were confirmed in all clones used for functional assays (i.e. CD14, CD115, CD49d, CD68, CD11b, CD163, HLA-DR). Of note, the makers CD116 and CD206, involved in GM-CSF signalling, were impaired in the original patient fibroblasts, but were rescued in the “corrected” patient-derived macrophages. The researchers then evaluated GM-CSF signalling by GM-CSF clearance assay. The gene-corrected macrophages cleared the GM-CSF in a comparable manner to wild-type cells, while no clearance was observed in the uncorrected original patient-derived differentiated macrophages. Downstream of GM-CSF signalling is STAT5, which becomes phosphorylated when activated. While the patient-uncorrected macrophages did not demonstrate any STAT5 phosphorylation due to the gene mutation, the gene-corrected macrophages showed a fully restored response. Likewise, PPARG (peroxisome proliferator-activated receptor gamma) gene expression is essential for alveolar macrophages, and it is downregulated in hPAP macrophages, but Dr Shima showed that it was entirely restored in gene-corrected macrophages. Cell proliferation upon stimulation of GM-CSF was also restored in gene-corrected macrophages. Proinflammatory signalling, as measured by tumour necrosis factor alpha release after exposure to lipopolysaccharide, indicated that the impaired activation of this response in the patient macrophages was fully restored, as was cholesterol clearance function using fluorescent cholesterol.
In conclusion, CRISPR/Cas9 genome editing successfully repaired the function of GM-CSF receptor in hPAP iPSCs. These results suggest that genome editing therapy is a promising strategy to further develop for treating hPAP patients in the future.
- Shima K, et al. A4004, ATS 2019, 17-22 May, Dallas, USA.
- Suzuki T, et al. Am J Respir Crit Care Med. 2014 Jan 15;189(2):183-93.
Posted on
Previous Article
« Sleep apnoea severity has a non-linear relationship with acute myocardial infarction risk Next Article
Dupilumab improves outcomes in patients with severe chronic rhinosinusitis with nasal polyps and comorbid asthma »
« Sleep apnoea severity has a non-linear relationship with acute myocardial infarction risk Next Article
Dupilumab improves outcomes in patients with severe chronic rhinosinusitis with nasal polyps and comorbid asthma »
Table of Contents: ATS 2019
Featured articles
Letter from the Editor
Interview with Prof. Christian Bergmann
Treatable Traits in Chronic Inflammatory Airway Disease: Back to Basics
Treatable traits in chronic inflammatory airway disease: back to basics
Critical Care Medicine
Distinguishing between 4 different subtypes of sepsis sets the stage for individualised treatment
Stem cell therapy in acute respiratory distress syndrome improves 28-day mortality
SPICE III trial: Early sedation with dexmedetomidine in critically ill patients
SAATELLITE trial: Suvratoxumab prevents ventilator-associated Staphylococcus Aureus pneumonia in intensive care unit patients
Sleep Medicine
Million-patient study reveals gaps in long-term adherence among various sub-populations
Sleep apnoea severity has a non-linear relationship with acute myocardial infarction risk
Obstructive sleep apnoea affects morning spatial navigational memory processing in asymptomatic older individuals
Pulmonary Vascular Disease and Interstitial Lung Disease
Nintedanib reduces lung function decline in systemic sclerosis-associated ILD
Pulmonary arterial hypertension: early treatment with selexipag most effective
Long-term safety and efficacy of recombinant human pentraxin-2 in patients with idiopathic pulmonary fibrosis
Infection
Dupilumab improves outcomes in patients with severe chronic rhinosinusitis with nasal polyps and comorbid asthma
Durability of culture conversion in patients receiving ALIS for treatment-refractory MAC lung disease
E-cigarette use disrupts normal immune response to viral infections, particularly in women
Paediatric Pulmonary Medicine
Bacterial pneumonia predicts ongoing lung problems in infants hospitalised for acute respiratory failure
Aspergillus and early cystic fibrosis lung disease: does it need to be treated?
COPD
CORTICO-COP trial: eosinophil-guided therapy reduces systemic corticosteroid exposure
A randomised controlled trial of a smoking cessation smartphone application
Benralizumab does not ameliorate COPD exacerbations (GALATHEA/TERRANOVA trials)
Aclidinium bromide delays COPD exacerbation without increased MACE risk
Bench-to-Bedside (Pre-Clinical)
Human lung organoids to study foetal RSV infection
CRISPR/Cas9 genome editing therapy of hereditary pulmonary alveolar proteinosis
Cilia diagnostics in primary ciliary dyskinesia
Tuberous sclerosis complex 2 may be a novel target in pulmonary arterial hypertension therapy
Related Articles
September 21, 2020
AstraZeneca says Tagrisso shown to slow lung cancer spreading to brain
October 30, 2022
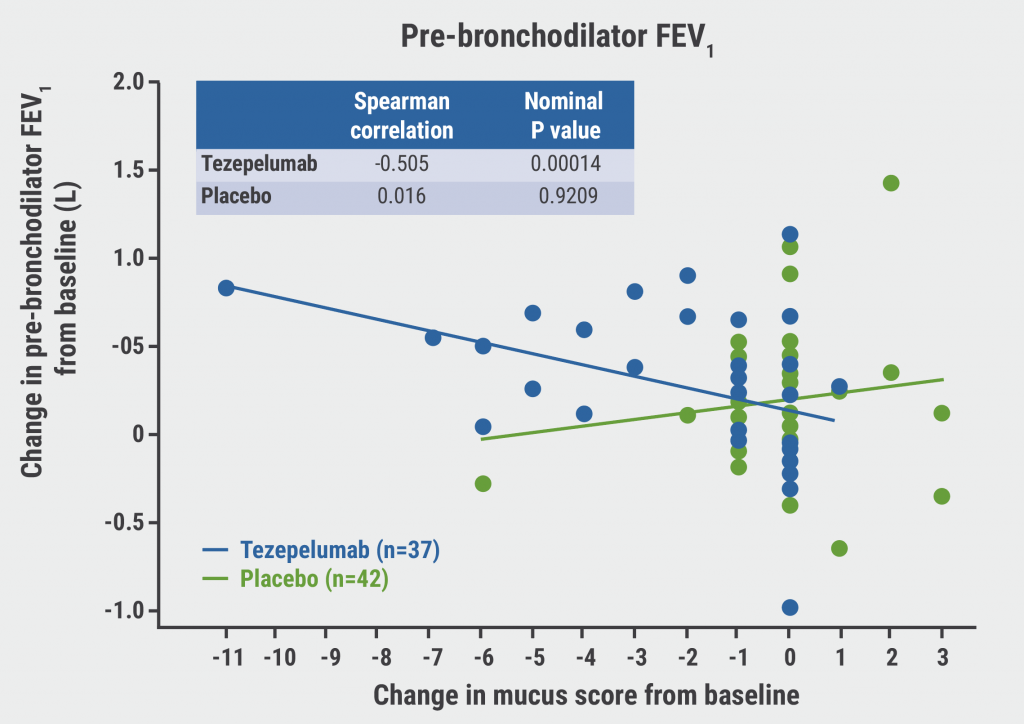
Tezepelumab in asthma: mucus plugging down, lung function up
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

