Sleep is thought to be critical for processing spatial memories, and spatial disorientation is one of the earliest hallmarks of cognitive dysfunction in Alzheimer disease. The investigators in this study wondered whether sleep disruption from OSA would negatively impact the processing of spatial navigational information in older asymptomatic individuals.
To this end, Dr Varga and colleagues recruited 42 cognitively normal older individuals (aged 66.5 ± 8 years) and had them explore a 3D computer generated spatial maze for 5 minutes, in addition to 3 timed trials (capped at 10 minutes each) to reach a target in the maze before and after polysomnographically recorded sleep. Subjects also completed a 20-minute psychomotor vigilance test (PVT) in the morning. Maze and PVT performance among 30 individuals without OSA (apnoea-hypopnoea index [AHI] 4% <5/hour) were compared with 12 individuals with OSA (AHI 4% ≥5/hour).
Median AHI 4% was 0.5/hour in subjects without OSA and 10.7/hour in subjects with OSA. N1 sleep was significantly increased in subjects with OSA (25.4% ± 4% in OSA vs 16.1% ± 1.5% in non-OSA, P=0.004) and N2 sleep was significantly decreased in subjects with OSA (41.5% ± 3% in OSA vs 48.4% ± 2% in non-OSA, P=0.034). No significant differences in N3 or REM sleep were observed. There were no significant differences in pre-sleep maze completion time, whereas post-sleep maze performance was significantly different between groups. Subjects without OSA continued to improve maze completion time on average across the 3 morning trials whereas subjects with OSA performed best on the first morning trial and performed worse on average with each subsequent trial (significant interaction between OSA group and morning trial number, P=0.016). There were no significant differences in mean reaction time (263 ms [IQR 233 ms-275 ms] in OSA vs 277 ms [IQR 251 ms-338 ms] in non-OSA, P=0.14) or number of lapses (2.5 lapses [IQR 0-4.5 lapses] in OSA vs 3 lapses [IQR 1-9.5 lapses] in non-OSA, P=0.3) on morning PVT.
The take-home message of the study was that cognitively normal older adults with mild OSA on average showed no deficits in morning vigilance, but nonetheless demonstrated significantly aberrant morning spatial navigation performance compared with individuals without OSA after equivalent spatial navigation encoding in the evening.
Dr Varga: “[The patient population] was a group of older people, average age was around 68 years old. One of the really interesting things is that these were people that were recruited from the community and did not intrinsically have any sleep complaints. So, they were not necessarily complaining that they had snoring or any other breathing issues with sleep apnoea. They were not complaining of any cognitive complaints, were not complaining of any sleepiness. We showed that, when we recruited this population, sleep apnoea is enormously prevalent, and when we kind of pushed the system and really tested them on this ability to remember space and spatial navigation, there was a deficit—even though they did not have any other issues.”
- Varga AW, et al. A7263, ATS 2019, 17-22 May, Dallas, USA.
Posted on
Previous Article
« Benralizumab does not ameliorate COPD exacerbations (GALATHEA/TERRANOVA trials) Next Article
Cilia diagnostics in primary ciliary dyskinesia »
« Benralizumab does not ameliorate COPD exacerbations (GALATHEA/TERRANOVA trials) Next Article
Cilia diagnostics in primary ciliary dyskinesia »
Table of Contents: ATS 2019
Featured articles
Letter from the Editor
Interview with Prof. Christian Bergmann
Treatable Traits in Chronic Inflammatory Airway Disease: Back to Basics
Treatable traits in chronic inflammatory airway disease: back to basics
Critical Care Medicine
Distinguishing between 4 different subtypes of sepsis sets the stage for individualised treatment
Stem cell therapy in acute respiratory distress syndrome improves 28-day mortality
SPICE III trial: Early sedation with dexmedetomidine in critically ill patients
SAATELLITE trial: Suvratoxumab prevents ventilator-associated Staphylococcus Aureus pneumonia in intensive care unit patients
Sleep Medicine
Million-patient study reveals gaps in long-term adherence among various sub-populations
Sleep apnoea severity has a non-linear relationship with acute myocardial infarction risk
Obstructive sleep apnoea affects morning spatial navigational memory processing in asymptomatic older individuals
Pulmonary Vascular Disease and Interstitial Lung Disease
Nintedanib reduces lung function decline in systemic sclerosis-associated ILD
Pulmonary arterial hypertension: early treatment with selexipag most effective
Long-term safety and efficacy of recombinant human pentraxin-2 in patients with idiopathic pulmonary fibrosis
Infection
Dupilumab improves outcomes in patients with severe chronic rhinosinusitis with nasal polyps and comorbid asthma
Durability of culture conversion in patients receiving ALIS for treatment-refractory MAC lung disease
E-cigarette use disrupts normal immune response to viral infections, particularly in women
Paediatric Pulmonary Medicine
Bacterial pneumonia predicts ongoing lung problems in infants hospitalised for acute respiratory failure
Aspergillus and early cystic fibrosis lung disease: does it need to be treated?
COPD
CORTICO-COP trial: eosinophil-guided therapy reduces systemic corticosteroid exposure
A randomised controlled trial of a smoking cessation smartphone application
Benralizumab does not ameliorate COPD exacerbations (GALATHEA/TERRANOVA trials)
Aclidinium bromide delays COPD exacerbation without increased MACE risk
Bench-to-Bedside (Pre-Clinical)
Human lung organoids to study foetal RSV infection
CRISPR/Cas9 genome editing therapy of hereditary pulmonary alveolar proteinosis
Cilia diagnostics in primary ciliary dyskinesia
Tuberous sclerosis complex 2 may be a novel target in pulmonary arterial hypertension therapy
Related Articles
January 29, 2024
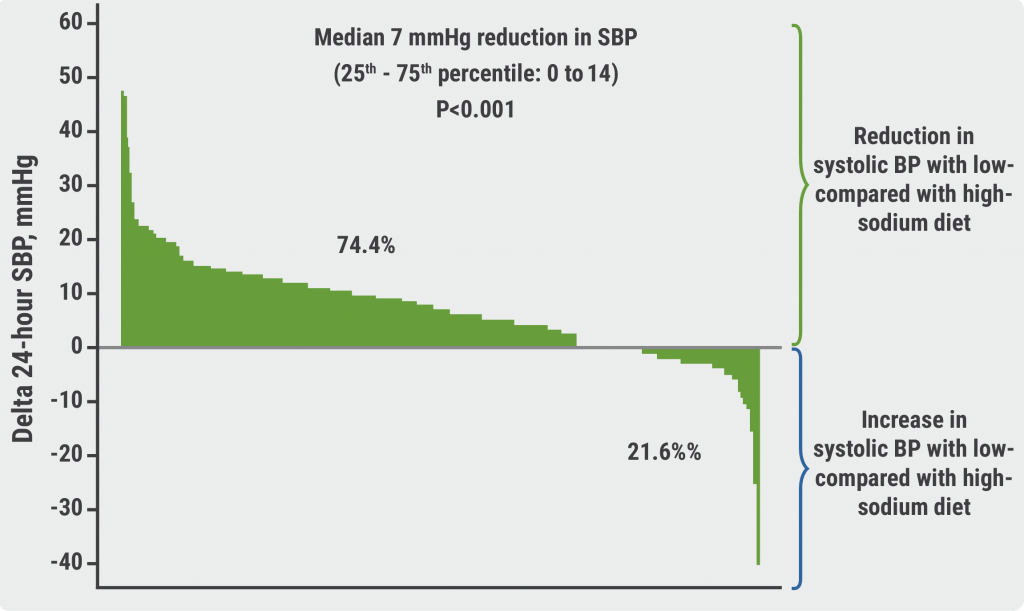
Sodium intake and blood pressure: new insights

June 6, 2019
Treatment patterns PAH have changed recently
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

