https://doi.org/10.55788/5c841567
Although current RA management possibilities entail fewer disease complications and better control of the inflammatory processes than before, D2T RA and prRA still pose a challenge in the medical treatment of those affected [1]. In 2021, EULAR defined criteria for D2T RA [2]. “In summary, it is the failure of at least 2 different types of b/ts DMARDs after failing conventional DMARDs in the presence of active or progressive disease,” Dr Paula David (University of Leeds, UK) informed [1]. By this broad definition, D2T RA applies to a very heterogeneous group of patients. The presented cross-sectional, single-centre study aimed not only to investigate the prevalence of D2T RA and prRA, but also to further characterise possible distinctive profiles according to the presence of disease activity on ultrasound.
Out of 1,591 reviewed medical records, 247 (15.5%) fulfilled the EULAR criteria of D2T RA. Among these, 40 patients were prRA, meaning they had failed all available b/ts DMARD classes. The demographic and clinical profiles of the 207 remaining D2T RA patients and those of prRA were largely similar. However, disease duration and time since first b/ts DMARD were significantly longer in the prRA group (P=0.008 and P=0.001, respectively). Also, the proportion of smoking differed significantly between both groups (4% [D2T RA] vs 20% [prRA], P=0.002). Significant differences between the 2 groups were also detected with a higher Disease Activity Score in 28 joints (DAS28), median C-reactive protein (CRP), and rate of patients with elevated CRP. A multivariate logistic regression identified 3 factors that were significantly associated with prRA. Exposure to b/ts DMARDS >9.5 years
Within 107 patients with information on a recent ultrasound, the investigators compared 2 different subgroups of D2T RA, both presenting a DAS28-CRP of ≥3.2: patients with persistent inflammatory refractory RA (PIRRA) had ultrasound-detected synovitis in at least 1 swollen joint, and in non-inflammatory refractory RA (NIRRA), the ultrasound-detected synovitis was absent in suspected clinically involved joints. “When comparing the PIRRA and NIRRA, we found that they also have very similar profiles, but the NIRRA group had higher BMI, obesity, and higher rates of fibromyalgia,” Dr David said. On the other hand, e.g. the swollen joint count, DAS28, and elevated CRP were higher in the PIRRA group. A swollen joint count >2 was associated with higher odds of PIRRA (OR 5.19; P<0.001), while each unit of higher BMI reduced the probability of PIRRA (OR 0.89; P<0.01). The figure summarises these study results (see Figure).
Figure: Poly-refractory RA: study findings in summary [1]
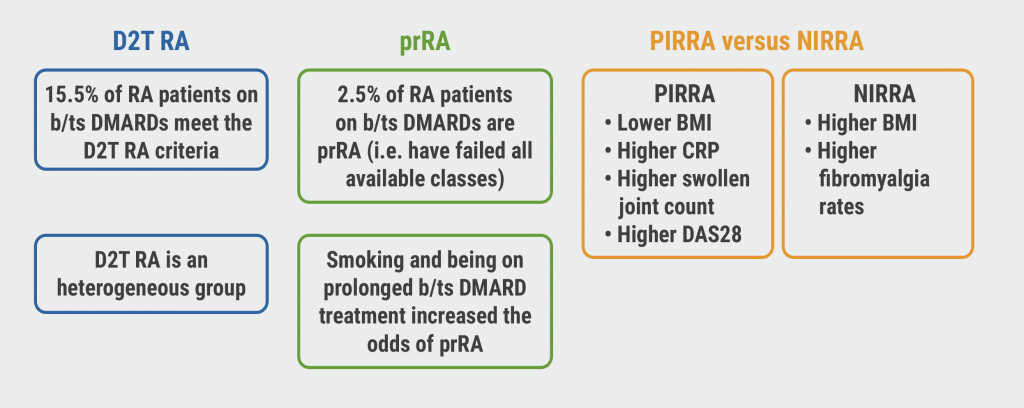
D2T, difficult-to-treat; RA, rheumatoid arthritis; prRA, poly-refractory RA; PIRRA, persistent inflammatory refractory RA; NIRRA, non-inflammatory refractory RA; b/ts DMARD, biologic/targeted synthetic disease- modifying antirheumatic drug; BMI, body mass index; CRP, C-reactive protein; DAS28, Disease Activity Score in 28 joints.
In her conclusion, Dr David underlined that it remains to be determined whether PIRRA patients benefit more from b/ts DMARD switching than NIRRA patients.
- David Real world “poly-refractory RA”: a rare but unmet clinical challenge. OP0134, EULAR 2023, 31 May–3 June, Milan, Italy.
- Nagy G, et Ann Rheum Dis. 2021;80:31-5.
Copyright ©2023 Medicom Medical Publishers
Posted on
Previous Article
« COBRA-Slim bio-induction: no benefit compared with the standard regimen Next Article
PsA patients: highest risk of developing NAFLD »
« COBRA-Slim bio-induction: no benefit compared with the standard regimen Next Article
PsA patients: highest risk of developing NAFLD »
Table of Contents: EULAR 2023
Featured articles
Late-breaking Oral Abstracts
Selective JAK1/TYK 2 inhibitor effective in patients with difficult-to-treat RA
Novel 2-drug combo improves treatment possibilities for patients with refractory gout
Dazodalibep improves dryness, fatigue, and pain in patients with Sjögren’s syndrome with a high symptom burden
COVID-19: Young adults with auto-immune diseases have different risks than their healthy counterparts
RA in 2023
Poly-refractory RA: not common, but still present
AI almost as successful as experts in predicting early RA
Worse self-management in patients with inflammatory arthritis in the presence of comorbid anxiety or depression
Disease activity-guided dose reduction may be a long-term option for stable RA
Cardiovascular safety of JAK inhibitors: reassuring results from a real-world study
Spondylarthropathies: New Developments
AxSpA: Adalimumab biosimilar equally effective as IL-17 inhibitor in hindering radiographic progression
Vascular inflammation may be characteristic of PsA
Obesity in PsA is increasingly affecting male patients
PsA patients: highest risk of developing NAFLD
What is Hot in Osteoarthritis
Lorecivivint shows long-term benefits for severe knee OA
Methotrexate lowers pain in inflammatory hand OA
Systemic Sclerosis: State of the Art
Targeted DMARDs advantageous in SSc patients with pre-capillary pulmonary hypertension
Osteoporosis: New Data
Drugs for osteoporosis: time to reach fracture risk reduction varies
Romosozumab: the new option for glucocorticoid-induced osteoporosis with high fracture risk?
Best of the Posters
Therapy with biological DMARDs shows no correlation with fracture risk in RA
Basic Science
In vitro and in vivo studies confirm the role of regulatory volume decrease
Related Articles
January 25, 2023
Top 14 Medical Innovations for 2022
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

