"The critical finding is that a simple, safe and noninvasive neuromodulation protocol is capable of rapidly reducing obsessive-compulsive symptoms in a nonclinical population, with the improvements sustaining for at least three months," lead author Shrey Grover of Boston University told Reuters Health by email. The study was published in Nature Medicine.
"Research into the clinical benefits of HD-tACS (theta band high-definition transcranial alternating current) in improving obsessive-compulsive symptoms is still in its infancy," he said "While our findings are promising,...larger studies examining such interventions in clinical populations with OCD and other disorders of compulsivity including gambling, addiction, and eating disorders will be needed."
"With additional research," he added, "we think such noninvasive neuromodulation protocols may prove to be useful for the clinician in treating obsessive-compulsive symptoms, particularly when traditional treatment approaches may be insufficient or impractical."
"The protocol involves application of weak electrical currents to the scalp using HD-tACS," Grover explained. "We manipulated the patterns of activity that are typically associated with reward processing in the brain which, when abnormal, can lead to obsessive-compulsive behavior."
Specifically, the researchers used a between-participants, double-blind, double-sham-controlled design in an involving a monetary reinforcement learning task. Sixty participants were randomly assigned to either the passive sham, active control (alpha frequency, 10 Hz) or personalized beta-gamma frequency (mean, 26.6 Hz) modulation group.
Personalized beta-gamma frequencies were determined during a pre-experiment EEG recording while participants learned to associate the stimuli with monetary rewards and losses.
Differences in behavioral choices were seen when comparing beta-gamma with sham, and beta-gamma with alpha, but not when comparing alpha with sham. This suggests, according to the authors, that beta-gamma modulation alone changed behavior.
Next, the researchers examined the effects of beta-gamma on obsessive-compulsive behaviors in a non-clinical group of 64 participants with obsessive-compulsive symptoms in the subclinical and clinical range. They established the endogenous reward-sensitive beta-gamma frequency for each participant, and assigned them to either the personalized beta-gamma group (mean 27.1 Hz) or the active control group undergoing alpha (10 Hz) modulation
HD-tACS targeted at the medial orbitofrontal cortex was applied for 30 minutes each day for five days; obsessive-compulsive behaviors were quantified using the Obsessive-Compulsive Inventory-Revised (OCI-R).
"Beta-gamma modulation induced a robust and long-lasting improvement in obsessive-compulsive behaviors attributed to stimulation artifacts," the authors state. Beta-gamma modulation selectively improved several subscales related to compulsivity, with significant group x time interactions for hoarding, ordering and obsessing behaviors.
Overall, participants with higher OCI-R scores at baseline showed greater reductions in obsessive-compulsive behaviors after beta-gamma modulation.
Dr. Ravi Shah, Medical Director, Psychiatry Faculty Practice at Columbia University Irving Medical Center in New York City, commented by email to Reuters Health, "The results are exciting and may lead to a new treatment for OCD."
Like Grover, he noted, "This study is small - i.e., 68 participants in the OCD experiment (who) were not diagnosed with OCD or any other psychiatric disorder. Before using this treatment with the public, we'd want to see larger clinical trials with people who have diagnosed OCD to replicate the findings."
Further, he added, "I did not see a discussion of any adverse effects or side effects from the treatment in this article. While the volunteers were healthy and the treatment is described as non-invasive, we'd want a full assessment of possible adverse reactions to ensure the treatment is safe."
SOURCE: https://go.nature.com/2NkF1ul Nature Medicine, online January 18, 2021
By Marilynn Larkin
Posted on
Previous Article
« Skin damage from UV light seen in sun-shielded skin Next Article
SAVR an option for many low-risk patients excluded from clinical trials »
« Skin damage from UV light seen in sun-shielded skin Next Article
SAVR an option for many low-risk patients excluded from clinical trials »
Related Articles
July 30, 2019
T-type-calcium channel modulator in essential tremor
July 30, 2019
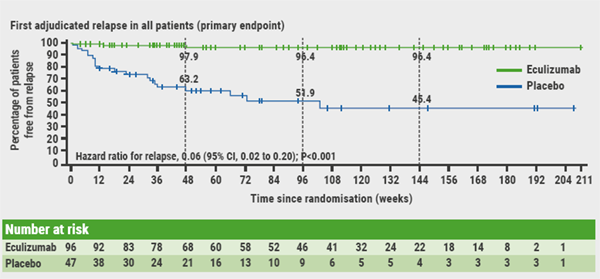
Three very promising new treatments of NMOSD
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

