Eculizumab in AQP4-IgG-positive NMOSD
At least two thirds of NMOSD cases are associated with aquaporin-4 antibodies (AQP4-IgG) and complement-mediated damage to the central nervous system. Eculizumab, a terminal complement inhibitor, reduced the risk of NMOSD relapse in patients with AQP4-IgG-positive NMOSD. In the phase 3 PREVENT trial, 143 adults were randomised to receive intravenous eculizumab or placebo. The mean annualised relapse rate (ARR) in the 2 years before enrolment was 1.99. It was permitted to continue stable-dose immunosuppressive therapy during the trial period; 76% of patients did.
The trial was stopped prematurely after the occurrence of 23 of the 24 prespecified adjudicated relapses, the primary endpoint (3% in the eculizumab group vs 43% in the placebo group; HR 0.06; P<0.001) [1]. Secondary outcomes included the adjudicated ARR (0.02 and 0.35 for eculizumab and placebo; rate ratio 0.04; P<0.001) and Expanded Disability Status Scale (EDSS) score (mean change -0.18 for eculizumab and +0.12 for placebo; least squares mean difference -0.29). So, no significant between-group difference in measures of disability progression was found. With respect to adverse events (AEs), upper respiratory tract infections and headaches were more common in the eculizumab group [1].
At ECTRIMS, Dr Dean Wingerchuk (Mayo Clinic, Rochester, United States) presented the combined long-term safety and effectiveness data from the PREVENT study and the ongoing open-label extension of PREVENT [2]. The 137 patients who were treated with eculizumab were followed for approximately 2 years (median 107.8 weeks). A high percentage (approximately 94%) of relapse-free patients remained relapse-free through 192 weeks [2]. Rates of AEs and serious AEs per 100 patient-years were 758.5 and 32.9, respectively. “In this long-term safety and effectiveness analysis, eculizumab was well tolerated”, Dr Wingerchuk concluded. “Reported AEs were consistent with the established safety profile of eculizumab in other indications” [2].
Inebilizumab in N-MOmentum trial
B-cell depletion may benefit patients with NMOSD. Inebilizumab is an anti-CD19 monoclonal antibody that depletes a broad range of B cells, including some CD20-negative antibody-secreting cells. In the phase 2/3 N-MOmentum trial, efficacy and safety of inebilizumab in reducing the risk of attacks and disability in adult patients with NMOSD were evaluated. At baseline, participants had an EDSS score of ≤8.0 in combination with either a history of ≥1 attack requiring rescue therapy in the year before screening or ≥2 attacks requiring rescue therapy in the 2 years before screening. In total, 230 patients were randomly allocated (3:1) to intravenous inebilizumab or placebo. The study population was 91% AQP4-IgG-positive, 91% female, and mean age was 43 years at study entry [3]. The primary endpoint was time to onset of an NMOSD attack, as determined by the adjudication committee.
Because of a clear demonstration of efficacy, the randomised controlled period was stopped before complete enrolment. Only 12% of participants receiving inebilizumab had an attack versus 39% receiving placebo (HR 0.272; P<0.0001). AEs occurred in 72% in the inebilizumab group and in 73% in the placebo group. Serious AEs occurred in 5% and 9% of the groups, respectively [3].
At ECTRIMS, Prof. Bruce Cree (University of California, San Francisco, USA) presented results from both the randomised controlled period and the open-label extension period of the N-MOmentum study [4]. He calculated that to prevent one attack, the number needed to treat for 6.5 months was 3.2 for the AQP4-IgG-positive group and 3.7 for the total population. On top of that, inebilizumab significantly reduced risk of worsening disability on EDSS and modified Rankin scale, number of new MRI lesions, and NMOSD-related hospitalisations. After one year, 85% of inebilizumab-treated patients were free of an NMOSD attack.
The most common AEs included urinary tract infection (19.6%), nasopharyngitis (12.9%), and infusion-related reactions (11.6%), which were most common with the first infusion. “The efficacy of inebilizumab was sustained at one year and was associated with an acceptable safety profile”, Prof. Cree concluded [4].
Satralizumab in SAkuraStar
In the immune pathology of NMOSD, the pro-inflammatory cytokine interleukin-6 (IL-6) is involved. Satralizumab is a monoclonal antibody that binds to the IL-6 receptor. In the SAkuraStar and SAkuraSky trials, satralizumab reduced relapse rate in patients with NMOSD, given as monotherapy and as add-on, respectively.
In SAkuraStar, 95 patients with NMOSD and ≥1 documented relapse in the year prior to screening, were randomised to satralizumab or placebo. Results were presented at ECTRIMS by Prof. Jeffrey Bennett (University of Colorado School of Medicine, Aurora, USA). The primary endpoint was time to first relapse. Overall, satralizumab reduced relapse risk by 55% compared with placebo (HR 0.45; P=0.018). The response was highly dependent on AQP4-IgG-serostatus, namely:
- In AQP4-IgG-seropositive patients, the HR was 0.26; and
- In AQP4-IgG-seronegative patients, the HR was 1.19 [5]
The proportions of AQP4-IgG-seropositive and -seronegative patients who were relapse-free at weeks 48 and 96 are listed in the Table. Prof. Bennett concluded that satralizumab was effective in reducing relapse risk in patients with NMOSD, particularly in AQP4-IgG-seropositive patients. Because this study was not powered for subgroup analyses, these results should be interpreted with caution [5].
Table. Efficacy results of satralizumab in SAkuraStar [5]

- Pittock SJ, et al. N Engl J Med. 2019;381:614-625.
- Wingerchuk DM, et al. ECTRIMS 2019, abstract 142.
- Cree BAC, et al. Lancet. 2019;394:1352-1363.
- Cree B, et al. ECTRIMS 2019, abstract 139.
- Bennett JL, et al. ECTRIMS 2019, abstract 141.
Posted on
Previous Article
« Less focus on quality of life in recent phase 3 trials Next Article
Late-breaking: Myelin-peptide coupled red blood cells »
« Less focus on quality of life in recent phase 3 trials Next Article
Late-breaking: Myelin-peptide coupled red blood cells »
Table of Contents: ECTRIMS 2019
Featured articles
Towards a Comprehensive Assessment of MS Course
Cognitive assessment in MS
Late-breaking: Role for CSF markers in autoimmune astrocytopathies
Targeted therapies for NMOSD in development
Monitoring and Treatment of Progressive MS
Challenges in diagnosing and treating progressive MS
Risk factors for conversion to secondary progressive MS
Transplantation of autologous mesenchymal stem cells
Sustained reduction in disability progression with ocrelizumab
Late-breaking: Myelin-peptide coupled red blood cells
Optimising Long-Term Benefit of MS Treatment
Induction therapy over treatment escalation
Treatment escalation over induction therapy
Influence of age on disease progression
Exposure to DMTs reduces disability progression
Predicting long-term sustained disability progression
Treatment response scoring systems to assess long term prognosis
Safety Assessment in the Post-Approval Phase
Use of clinical registries in phase 4 of DMT
Genes, environment, and safety monitoring in using registries
Risk of hypogammaglobulinemia and rituximab
Determinants of outcomes for natalizumab-associated PML
Serum immunoglobulin levels and risk of serious infections
EAN guideline on palliative care
Pregnancy in the Treatment Era
The maternal perspective: when to stop/resume treatment and risks for progression
Foetal/child perspective: risks related to drug exposure and breastfeeding
Patient awareness about family planning represents a major knowledge gap
Late-breaking: Continuation of natalizumab or interruption during pregnancy
Related Articles
August 18, 2021
Typing behaviour to remotely monitor clinical MS status
November 25, 2020
Disease activity during pregnancy in a modern MS cohort
November 18, 2024
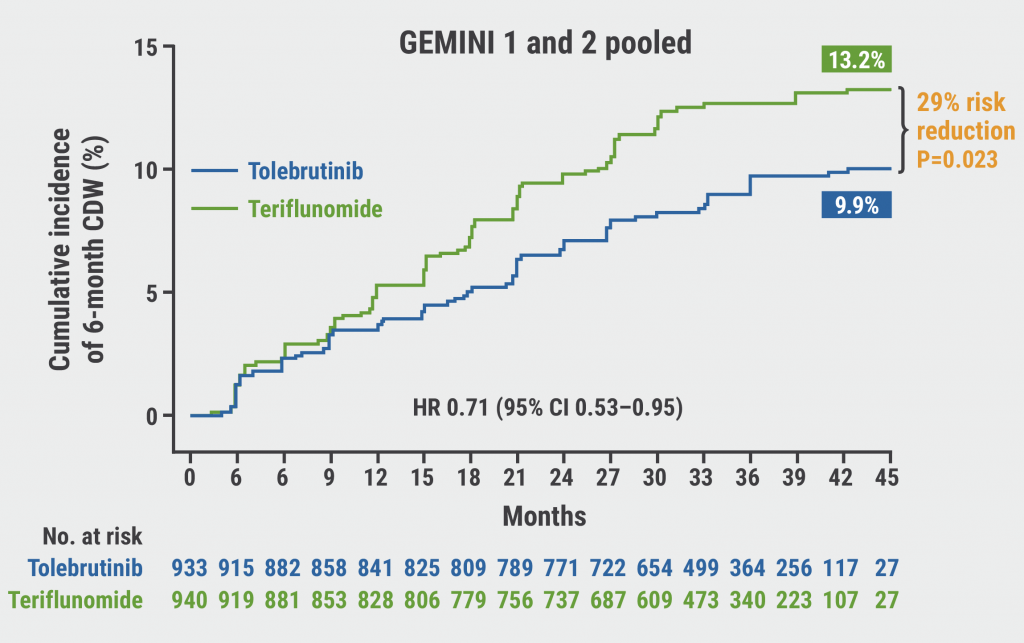
Tolebrutinib slows disability worsening in relapsing MS
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

