The interface of the Swedish MS registry shows the “whole evolution of a certain patient”, Olsson continued, “such as the EDSS course and the different drugs given.” This has led to a widespread use of these rates in Sweden, with 17,397 of 20,500 current MS patients included (85% coverage). The data are used for research in genetics, neuroimmunology, epidemiology, post-marketing follow-up, and biobanks [1]. Subsequently, Prof. Olsson mentioned some selected examples of research projects using the Swedish MS registry as a platform. After the introduction of natalizumab and knowing the influence of JC virus on progressive multifocal leukoencephalopathy (PML) risk, he started the Immunomodulation and MS Epidemiology (IMSE) studies. “Since then, a lot of new drugs have come to the market, so post-marketing surveillance was warranted. Furthermore, several genetics, lifestyle, and environmental factors in MS (EIMS) studies are based on the Swedish data.”
Genetics, lifestyle, and environmental factors
The pathophysiological cascade of MS is characterised by many factors. “We need precise knowledge on causes of MS to provide prevention and more precise therapy. This has been a neglected area”, according to Prof. Olsson. This includes risk genes, lifestyle, and environmental factors, and the interactions between them [2]. Lifestyle and environmental factors have a modest influence (odd ratios of approximately 1.5-2), although their influence is mostly higher compared to the influence of non-HLA genes (ORs of approximately 1.1-1.2). Some factors act during adolescence and early adulthood, such as Epstein-Barr virus (EBV), obesity, brain concussion, and disturbed diurnal rhythm. Many factors interact with MS risk genes; all factors can be argued to act on the immune system.
Further research on the aetiology of MS is warranted to achieve prevention and more selective therapy. Perhaps there should be new emphasis on the adaptive immunity, including ways to define specificities and functions to auto-aggressive T and B cells. The combination of genetics and epidemiology may lead us into testable hypotheses, as exemplified by the interaction between smoking and HLA genes. Thus, combined studies are warranted. Upcoming genetics research should take environmental exposures into account; upcoming epidemiology research should take genetics into account.
- Hillert J, Stawiarz L. Acta Neurol Scand. 2015;132:11-9.
- Olsson T, et al. Nat Rev Neurol. 2017;13:25-36.
Posted on
Previous Article
« Talazoparib + low-dose temozolomide seems promising in ES-SCLC Next Article
Risk factors for conversion to secondary progressive MS »
« Talazoparib + low-dose temozolomide seems promising in ES-SCLC Next Article
Risk factors for conversion to secondary progressive MS »
Table of Contents: ECTRIMS 2019
Featured articles
Towards a Comprehensive Assessment of MS Course
Cognitive assessment in MS
Late-breaking: Role for CSF markers in autoimmune astrocytopathies
Targeted therapies for NMOSD in development
Monitoring and Treatment of Progressive MS
Challenges in diagnosing and treating progressive MS
Risk factors for conversion to secondary progressive MS
Transplantation of autologous mesenchymal stem cells
Sustained reduction in disability progression with ocrelizumab
Late-breaking: Myelin-peptide coupled red blood cells
Optimising Long-Term Benefit of MS Treatment
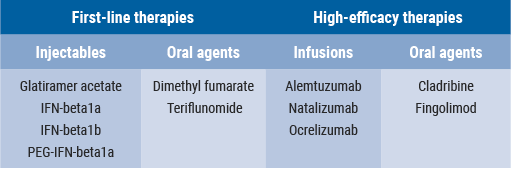
Induction therapy over treatment escalation
Treatment escalation over induction therapy
Influence of age on disease progression
Exposure to DMTs reduces disability progression
Predicting long-term sustained disability progression
Treatment response scoring systems to assess long term prognosis
Safety Assessment in the Post-Approval Phase
Use of clinical registries in phase 4 of DMT
Genes, environment, and safety monitoring in using registries
Risk of hypogammaglobulinemia and rituximab
Determinants of outcomes for natalizumab-associated PML
Serum immunoglobulin levels and risk of serious infections
EAN guideline on palliative care
Pregnancy in the Treatment Era
The maternal perspective: when to stop/resume treatment and risks for progression
Foetal/child perspective: risks related to drug exposure and breastfeeding
Patient awareness about family planning represents a major knowledge gap
Late-breaking: Continuation of natalizumab or interruption during pregnancy
Related Articles
November 8, 2019
Risk of hypogammaglobulinemia and rituximab
November 8, 2019
Transplantation of autologous mesenchymal stem cells
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

