CHB is one of the clinical manifestations of neonatal lupus syndrome [2]. It is associated with a 17.5% mortality and 70% requirement of permanent pacing [3]. The disease is induced by a placental transport of maternal anti-SSA/Ro antibodies [2]. Women carrying these antibodies may have systemic lupus erythematosus, Sjögren syndrome, or other connective tissue diseases, or may be completely healthy at the time of giving birth [2].
“CHB affects an estimated 2% of pregnancies among women who have anti-SSA/Ro antibodies who have never been pregnant or have never had an affected child. It appears maternal health accompanying the production of the candidate autoantibodies is not a risk factor for foetal disease, since many mothers whose foetuses develop cardiac injury are asymptomatic and often learn of anti-SSA/Ro antibodies solely based on disease in their children,” explained Prof. Peter Izmirly (New York University School of Medicine, USA). Once an affected child is born, the risk for the next child rises dramatically and has been found to climb up to 18% for subsequent babies to be born suffering from CHB [3]. Given the high mortality of CHB, the optimal approach is prevention.
The PATCH study was performed to find out if hydroxychloroquine could lower recurrence rates of CHB below the historical mark of 18%. The single-arm phase 2 trial was designed in 2 stages to take an early study stop into consideration in case of inefficacy of hydroxychloroquine. Stage 1 included 19 and stage 2 an additional 35 currently pregnant women who were all anti-SSA/Ro positive and had given birth to a child with CHB before. Treatment was initiated with 400 mg of hydroxychloroquine daily by 10 weeks of gestation. Surveillance during pregnancy was performed by sequential echocardiograms for PR intervals, advanced block, and cardiomyopathy. Furthermore, compliance was checked by measurement of hydroxychloroquine levels every trimester and within the cord blood. Treatment adherence was confirmed in 98% of the mothers. Primary outcome was second-/third-degree block in utero or at birth.
In the first stage, only 2 children were diagnosed with CHB, and so the trial proceeded to stage 2 in which 2/35 enrolled mothers gave birth to a child with CHB. Per intention-to-treat analysis of both stages, in 7.4% (4/54) an outcome with CHB was found, leading to a significant result in favour of hydroxychloroquine (P=0.02). “Our group has previously reported in a historical cohort that the use of hydroxychloroquine may be associated with a reduced recurrence rate of CHB, but this is the first prospective study to confirm those findings,” Prof. Izmirly pointed out. “Given the morbidity and mortality associated with the disease and the relative safety of hydroxychloroquine use during pregnancy, a treating physician should consider using hydroxychloroquine to reduce the risk of CHB in a mother who has had a previously affected child,” he concluded.
- Izmirly P, et al. Abstract 1761. ACR 2019. 8-13 November, Atlanta (GA/USA).
- Zuppa AA, et al. Autoimmun Rev. 2017;16:427-432.
- Izmirly P, et al. Circulation. 2011;124:1927-35.
Posted on
Previous Article
« Opioids: no quality of life benefits for OA patients Next Article
Calcium pyrophosphate deposition disease: an independent risk factor for cardiovascular complications »
« Opioids: no quality of life benefits for OA patients Next Article
Calcium pyrophosphate deposition disease: an independent risk factor for cardiovascular complications »
Table of Contents: ACR 2019
Featured articles
Late-Breaking Abstracts
Lowest risk of infection after therapy with an IL-12/IL-23 blocker
Calcium pyrophosphate deposition disease: an independent risk factor for cardiovascular complications
Proteome abnormalities improve prediction of RA development
RA patients in remission benefit from continued therapy with conventional DMARDs
Selective IL-23 blocker shows remarkable efficacy in patients with psoriatic arthritis
Corticosteroid therapy in GCA: higher platelets – lower relapse rate
Spotlight on Rheumatoid Arthritis
Filgotinib promising in RA patients naïve to methotrexate
Sustained efficacy of monotherapy with upadacitinib after 48 weeks
Biologics show similar activity in patients with elderly-onset RA
Tocilizumab outperforms rituximab in RA patients with low level of synovial B cell infiltration
Treatment decisions should not be guided by ultrasound findings
Cancer treatment with checkpoint inhibitors in RA patients?
What is Hot in Systemic Lupus Erythematosus
Anifrolumab succeeds in second phase 3 trial in SLE
Depression closely related to fatigue in SLE patients
Spondyloarthritis – The Beat Goes On
Psoriasis onset determines sequence of symptoms
Higher psychiatric comorbidity in women with PsA
JAK1 inhibition shows remarkable efficacy in AS
CARDAS study shows increased prevalence of cardiac valvular disorders in AS patients
Osteoarthritis – State-of-the-Art
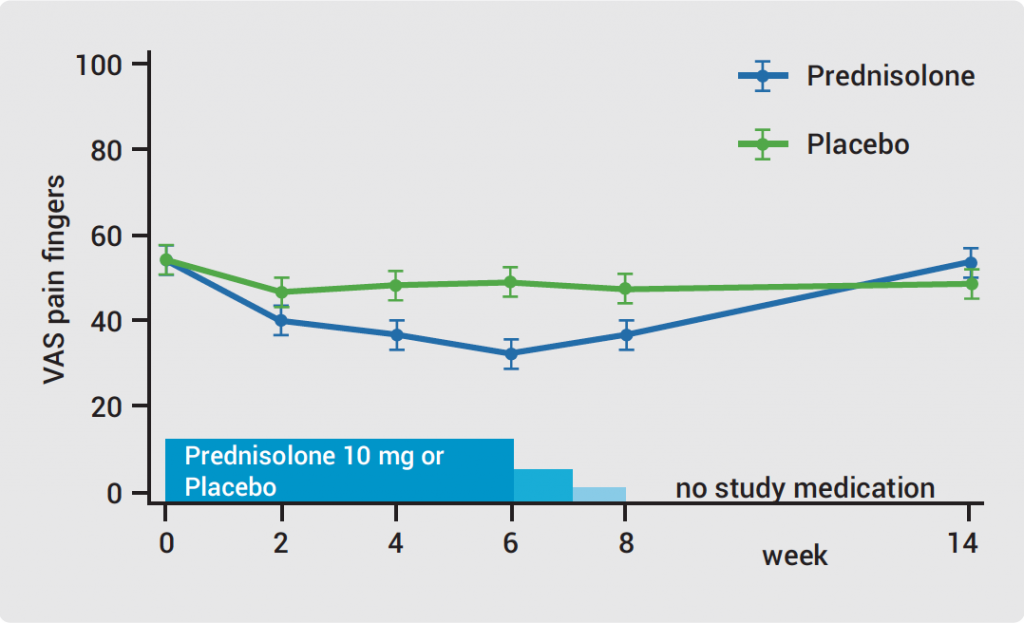
Hand OA: low-dose corticosteroids improve symptoms
Opioids: no quality of life benefits for OA patients
Walking speed is a predictor of mortality in patients with knee OA
Reproductive Issues in Rheumatic Disease
Few serious infections in offspring with exposure to non-TNFi biologics or tofacitinib
Prevention of congenital heart block may be possible with hydroxychloroquine
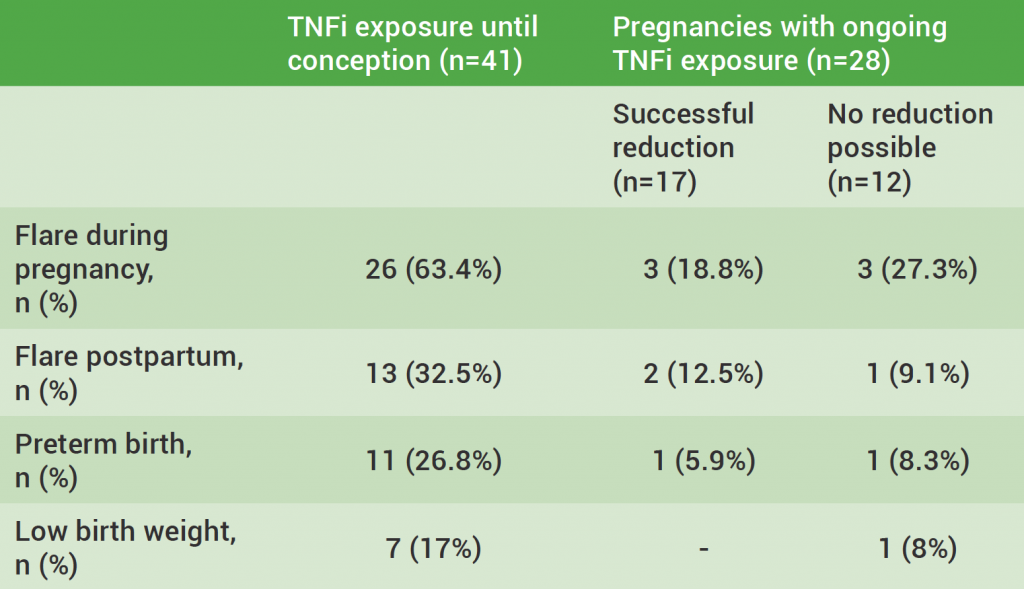
TNFi for RA during pregnancy – to stop or not to stop?
Vasculitis – Novel Treatment Modalities
Rituximab maintenance superior to azathioprine in ANCA-associated vasculitis
Prolonged remission after stop of tocilizumab for patients with giant cell arteritis
Best of the Posters
Antifibrotic therapy slows disease progression independent of corticosteroid use
Fibromyalgia patients often experienced abuse in childhood
Related Articles
February 4, 2020
Hand OA: low-dose corticosteroids improve symptoms
February 4, 2020
Lowest risk of infection after therapy with an IL-12/IL-23 blocker
February 4, 2020
TNFi for RA during pregnancy – to stop or not to stop?
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

