Anifrolumab is a human monoclonal antibody that binds the type 1 interferon receptor subunit 1. Type 1 interferons play a key role in the pathogenesis of systemic lupus erythematosus (SLE), as these cytokines are involved in the inflammatory pathways [2]. Between 60% and 80% of adults with SLE have an increased type 1 interferon gene signature, which has been shown to correlate with disease activity [3,4]. Therefore, type 1 interferons are an interesting target for the therapy of SLE. In the TULIP 2 study, 180 patients with moderate-to-severe SLE were randomly assigned to receive anifrolumab (300 mg intravenously) or placebo every 4 weeks for 48 weeks. The primary endpoint of the trial was a difference in the BILAG-Based Composite Lupus Assessment (BICLA).
At week 52, 47.8% of 180 patients had achieved BICLA response, compared with 31.5% of 182 patients assigned to placebo (P=0.0013). Even more pronounced was the comparison between anifrolumab and placebo in the group of patients who scored high on tests for the type 1 interferon gene signature (45.9% vs 27.5% in the placebo group). “Separation between the treatment arms occurred early and was maintained across the duration of the trial,” said Prof. Eric Morand (Monash University, Melbourne, Australia) during the presentation of the study. Anifrolumab also showed superiority in a couple of secondary endpoints: 51.5% of anifrolumab patients receiving oral corticosteroids (OCS) ≥10 mg achieved a sustained reduction in OCS use compared with 30.2% of patients on placebo. Additionally, 49% of patients receiving anifrolumab with moderate-to-severe skin disease experienced improved skin manifestations at week 12, compared with 25% of patients receiving placebo. Skin manifestations were measured by the Cutaneous Lupus Erythematosus Disease Area and Severity Index (CLASI). The improvement of skin symptoms was sustained for the remaining duration of the trial.
TULIP 1 trial fails to achieve primary endpoint
In contrast to the results of the TULIP 2 trial, anifrolumab failed to be superior to placebo with regard to an SLE responder index (SRI)-4 response at 1 year which emerged from the TULIP 1 trial that was also presented during the meeting [5]. This endpoint was achieved by 36% of 180 patients treated with anifrolumab compared with 40% of placebo patients, a nonsignificant difference. Similar to the TULIP 2 study, there were hints to activity with regard to BICLA response, sustained OCS dose reduction, and organ-specific measures of skin and joint responses, although the statistical significance of these differences was not formally assessed.
According to Prof. Richard Furie (Northwell Health, New York, USA), the difference in the outcome of the TULIP 1 and TULIP 2 trials might be due to differences in the primary endpoint: the SRI-4 is based on the Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K), which requires complete resolution of a manifestation before that item’s score will change. By contrast, BICLA is based on improvements in BILAG-2004, which registers both graded and complete improvements within an organ domain and, therefore, is more sensitive.
The safety and tolerability findings in TULIP 1 and TULIP 2 were consistent with the known profile of anifrolumab [1-3]. There were more commonly reported cases of herpes zoster in patients on anifrolumab compared with placebo (TULIP 1: 5.6% vs 1.6%; TULIP 2: 7.2% vs 1.1%). However, most cases were mild to moderate in severity, all cases responded to antiviral therapy and none required discontinuation of treatment. The therapy of SLE including the historical use of rituximab has fallen fowl of outcome measures and hopefully the TULIP programme will accelerate outcome measure optimisation towards novel therapy development.
- Morand E et al. Abstract L17. ACR 2019, 9-13 November, Atlanta (GA/USA).
- Furie R et al. Arthritis Rheumatol 2017;69;376-386.
- Lauwerys BR et al. Rheumatology (Oxford) 2014;53;1369-1376.
- Crow MK. J Immunol 2014;192;5459-68.
- Furie R et al. Abstract 1763. ACR 2019, 9-13 November, Atlanta (GA/USA).
Posted on
Previous Article
« Lowest risk of infection after therapy with an IL-12/IL-23 blocker Next Article
Letter from the Editor »
« Lowest risk of infection after therapy with an IL-12/IL-23 blocker Next Article
Letter from the Editor »
Table of Contents: ACR 2019
Featured articles
Late-Breaking Abstracts
Lowest risk of infection after therapy with an IL-12/IL-23 blocker
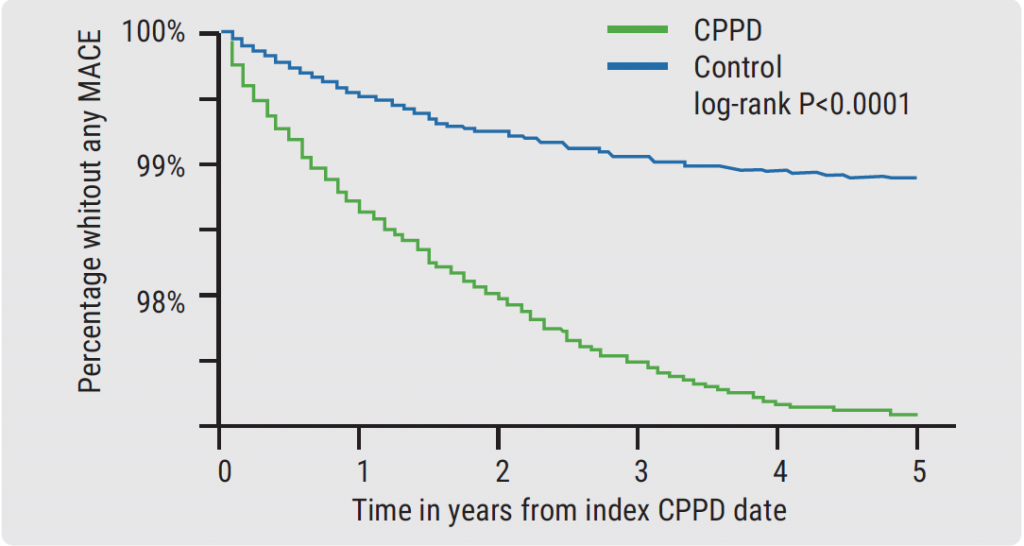
Calcium pyrophosphate deposition disease: an independent risk factor for cardiovascular complications
Proteome abnormalities improve prediction of RA development
RA patients in remission benefit from continued therapy with conventional DMARDs
Selective IL-23 blocker shows remarkable efficacy in patients with psoriatic arthritis
Corticosteroid therapy in GCA: higher platelets – lower relapse rate
Spotlight on Rheumatoid Arthritis
Filgotinib promising in RA patients naïve to methotrexate
Sustained efficacy of monotherapy with upadacitinib after 48 weeks
Biologics show similar activity in patients with elderly-onset RA
Tocilizumab outperforms rituximab in RA patients with low level of synovial B cell infiltration
Treatment decisions should not be guided by ultrasound findings
Cancer treatment with checkpoint inhibitors in RA patients?
What is Hot in Systemic Lupus Erythematosus
Anifrolumab succeeds in second phase 3 trial in SLE
Depression closely related to fatigue in SLE patients
Spondyloarthritis – The Beat Goes On
Psoriasis onset determines sequence of symptoms
Higher psychiatric comorbidity in women with PsA
JAK1 inhibition shows remarkable efficacy in AS
CARDAS study shows increased prevalence of cardiac valvular disorders in AS patients
Osteoarthritis – State-of-the-Art
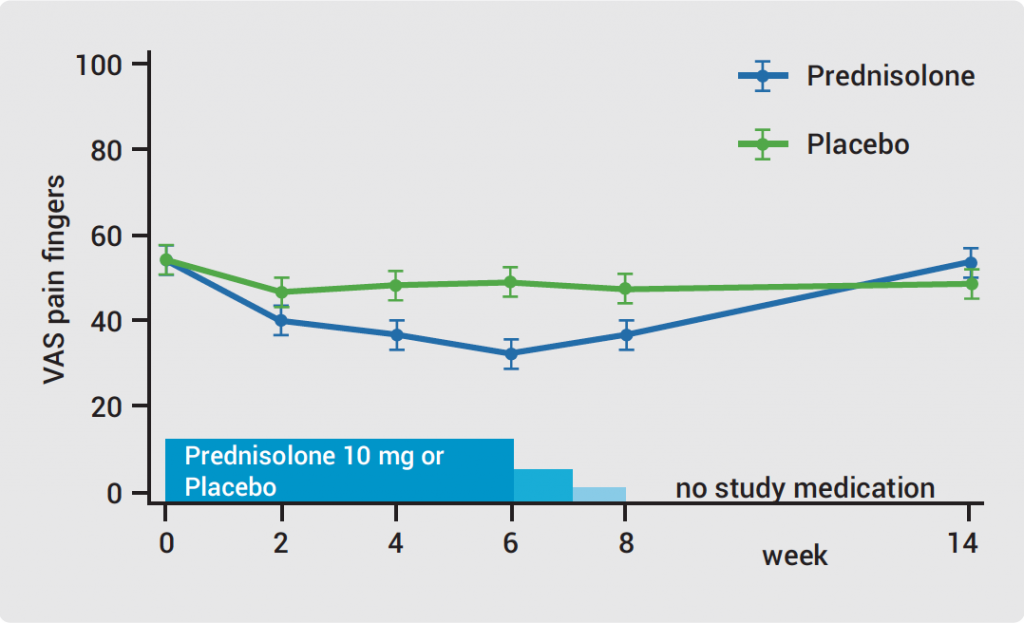
Hand OA: low-dose corticosteroids improve symptoms
Opioids: no quality of life benefits for OA patients
Walking speed is a predictor of mortality in patients with knee OA
Reproductive Issues in Rheumatic Disease
Few serious infections in offspring with exposure to non-TNFi biologics or tofacitinib
Prevention of congenital heart block may be possible with hydroxychloroquine
TNFi for RA during pregnancy – to stop or not to stop?
Vasculitis – Novel Treatment Modalities
Rituximab maintenance superior to azathioprine in ANCA-associated vasculitis
Prolonged remission after stop of tocilizumab for patients with giant cell arteritis
Best of the Posters
Antifibrotic therapy slows disease progression independent of corticosteroid use
Fibromyalgia patients often experienced abuse in childhood
Related Articles
February 4, 2020
Hand OA: low-dose corticosteroids improve symptoms
February 4, 2020
Proteome abnormalities improve prediction of RA development
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

