Having comorbidity of autoimmune disease generally leads to the exclusion of oncologic trials with ICI, as there are worries about more immune-related adverse events (irAEs) [1]. “However, patients with autoimmune diseases have the potential to benefit from the use of these therapies,” commented Dr Sabina Sandigursky (New York University Langone Medical Center, USA).
The reported study investigated 84 patients with known autoimmunity who had been treated with anti-CTLA-4 and PD-1 for their cancer from 2011-2018. There were 22 patients of this group who suffered from RA. The majority was female (73%), median age was 67. When starting ICI, 73% of the patients were on immunomodulatory treatment, including 36% taking corticosteroids and 32% methotrexate. With regard to cancer subtypes, 32% each were diagnosed with melanoma or non-small cell lung cancer. Primary trial endpoints were incidences of irAEs and RA flares.
IrAEs occurred in 32% of the RA patients, but only 9% were of severe nature. RA flares were observed in 55% of patients, and ICI treatment had to be entirely stopped in 1 patient; short-term discontinuation was necessary in 23%. Depending on the drug that was administered, the rate of serious irAEs in patients without autoimmunity ranged from 7-30%. Flare treatment was performed with corticosteroids in 75% of the cases. In general, toxicity occurred in 32% of patients, the most frequent being dermatitis (18%) and colitis (14%). The overall survival for RA patients under ICI was 10.5 months after ICI initiation.
“Our data suggests that patients with RA may be treated with immunotherapy and attain rates of response that are similar to the general population with a 50% flare rate,” said Dr Sandigursky. “If validated in prospective clinical trials, this study’s findings may open new treatment options for patients with autoimmune diseases and concurrent malignancy. A co-management approach between the oncologist and rheumatologist can help recognise and treat immunotherapy-related toxicities if they do arise.” Rheumatologists and oncologists have reached an interesting therapeutic crossroad and need to consider the impact of RA-directed therapy on overall tumour survival, as steroids and disease-modifying antirheumatic drugs (DMARDs) might impact anti-tumoral immunity [2].
- Efuni E, et al. Abstract 1339. ACR 2019. 8-13 November, Atlanta (GA/USA).
- McGonagle D, et al. Autoimmun Rev. 2019 Dec 12:102456.
Posted on
Previous Article
« Fibromyalgia patients often experienced abuse in childhood Next Article
Depression closely related to fatigue in SLE patients »
« Fibromyalgia patients often experienced abuse in childhood Next Article
Depression closely related to fatigue in SLE patients »
Table of Contents: ACR 2019
Featured articles
Late-Breaking Abstracts
Lowest risk of infection after therapy with an IL-12/IL-23 blocker
Calcium pyrophosphate deposition disease: an independent risk factor for cardiovascular complications
Proteome abnormalities improve prediction of RA development
RA patients in remission benefit from continued therapy with conventional DMARDs
Selective IL-23 blocker shows remarkable efficacy in patients with psoriatic arthritis
Corticosteroid therapy in GCA: higher platelets – lower relapse rate
Spotlight on Rheumatoid Arthritis
Filgotinib promising in RA patients naïve to methotrexate
Sustained efficacy of monotherapy with upadacitinib after 48 weeks
Biologics show similar activity in patients with elderly-onset RA
Tocilizumab outperforms rituximab in RA patients with low level of synovial B cell infiltration
Treatment decisions should not be guided by ultrasound findings
Cancer treatment with checkpoint inhibitors in RA patients?
What is Hot in Systemic Lupus Erythematosus
Anifrolumab succeeds in second phase 3 trial in SLE
Depression closely related to fatigue in SLE patients
Spondyloarthritis – The Beat Goes On
Psoriasis onset determines sequence of symptoms
Higher psychiatric comorbidity in women with PsA
JAK1 inhibition shows remarkable efficacy in AS
CARDAS study shows increased prevalence of cardiac valvular disorders in AS patients
Osteoarthritis – State-of-the-Art
Hand OA: low-dose corticosteroids improve symptoms
Opioids: no quality of life benefits for OA patients
Walking speed is a predictor of mortality in patients with knee OA
Reproductive Issues in Rheumatic Disease
Few serious infections in offspring with exposure to non-TNFi biologics or tofacitinib
Prevention of congenital heart block may be possible with hydroxychloroquine
TNFi for RA during pregnancy – to stop or not to stop?
Vasculitis – Novel Treatment Modalities
Rituximab maintenance superior to azathioprine in ANCA-associated vasculitis
Prolonged remission after stop of tocilizumab for patients with giant cell arteritis
Best of the Posters
Antifibrotic therapy slows disease progression independent of corticosteroid use
Fibromyalgia patients often experienced abuse in childhood
Related Articles

September 17, 2021
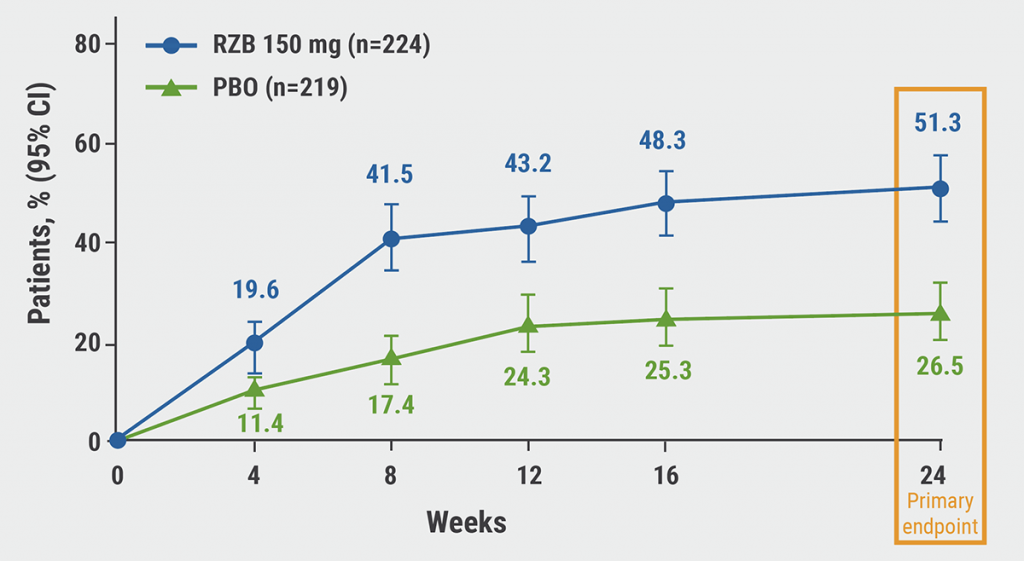
Selective TYK2 inhibitor effective in moderate-to-severe plaque psoriasis
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

