Neuroinflammation is a maladaptive brain response commonly ignited in human epileptogenic brain regions and is clearly involved in animal models of epilepsy, Prof. Vezzani explained. Experimental studies in animal models showed that -if not adequately controlled- neuroinflammation is involved in the pathogenesis of seizures, neuronal cell loss, and neurological comorbidities. Neuroinflammation has now been related to several types of human epilepsy:
- temporal lobe epilepsy with or without hippocampal sclerosis;
- malformations of cortical development, i.e. hemimegaloencephaly (HME), focal cortical dysplasia (FCD) type II, tuberous sclerosis;
- Rasmussen's encephalitis;
- febrile infection-related epilepsy syndrome (FIRES);
- acute symptomatic seizures and status epilepticus;
- neonatal febrile seizures;
- acquired epilepsies;
- absence seizures and progressive myoclonus epilepsy of Unverricht-Lundborg type (EPM1).
Insights into the dynamics of neuroinflammation in epilepsy has generated several potential cellular and molecular targets for developing new drugs, or for repurposing of available anti-inflammatory drugs, acting on key pathogenic mechanisms. Inflammatory mediators such as interleukin (IL)-1β, tumour necrosis factor (TNF), high mobility group box 1, transforming growth factor-β, and prostaglandins can alter neuronal, glial, and blood–brain barrier functions by activating transcriptional and post-translational mechanisms in brain cells. Proof-of-concept target-specific anti-inflammatory interventions in animal models of epilepsy have reported anti-ictogenic, anti-epileptogenic, and disease-modifying therapeutic effects. Prof. Vezzani specifically mentioned the IL-1 receptor antagonist anakinra, which has been administered to several patients [2].
Moreover, blood inflammatory mediators and molecular imaging of neuroinflammation are providing potential diagnostic, prognostic, and predictive biomarkers for epilepsy which are instrumental for patient stratification in future clinical studies.
1. Vezzani A. EAN 2019, PLEN03_1.
2. Jyonouchi H, et al. J Clin Cell Immunol 2016;7:5.
Posted on
Previous Article
« Thrombo-inflammation during ischaemia/reperfusion Next Article
Switch to sarilumab from adalimumab is efficacious and safe »
« Thrombo-inflammation during ischaemia/reperfusion Next Article
Switch to sarilumab from adalimumab is efficacious and safe »
Table of Contents: EAN 2019
Featured articles
Letter from the Editor
Alzheimer’s Disease and other Dementias
A necessary shift of focus to the earlier stages of Alzheimer’s
Antipsychotics increase mortality regardless of comorbidity
Epilepsy
Neuroinflammatory pathways as biomarkers and treatment targets
Long-term effect of recurrent febrile seizures
Migraine
The role of neurogenic inflammation in migraine
Multiple Sclerosis
Treating MS from disease onset
Randomised and observational studies comparing treatments
Autologous haematopoietic stem cell transplantation
Neuromuscular Disorders
Parkinson's Disease and other Movement Disorders
Inflammation may change the course of Parkinson’s disease
Opicapone: follow-up on the BIPARK I and II trials
Epigallocatechin gallate does not modify MSA progression
Stroke
Thrombo-inflammation during ischaemia/reperfusion
Related Articles
November 8, 2021
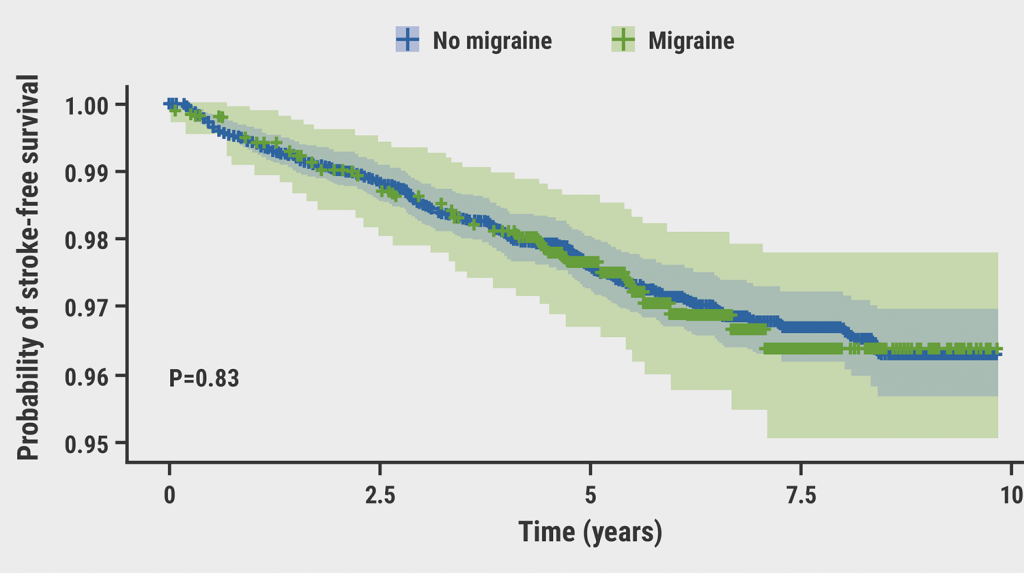
Migraine may not be a risk factor for stroke
February 9, 2022
Endovascular therapy found effective for larger cerebral infarctions
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

