Adults with a proven SARS-CoV-2 infection, symptomatic or asymptomatic COVID-19, and without rheumatic disease prior to infection were included. Dr Alessia Alunno (University of Perugia, Italy) presented the results [1]. Glucocorticoid therapy in addition to standard of care (5 randomised clinical trials [RCTs]) showed a reduced mortality rate compared with standard treatment for oxygen-receiving (RR 0.89; 95% CI 0.79–1.00) and mechanically ventilated (RR 0.71; 95% CI 0.58–0.86) COVID-19 patients in the large RCT RECOVERY (NCT04381936; n=6,425). In contrast, the use of glucocorticoids in patients not receiving supplemental oxygen increased the mortality rate (RR 1.27; 95% CI 1.00–1.61). Older age of COVID-19 patients (>60 years) was associated with reduced mortality when they were treated with glucocorticoids (RR 0.75; 95% CI 0.56–1.01).
Five RCTs on tocilizumab did not demonstrate mortality benefits in COVID-19 patients. However, the largest included trial, REMAP-CAP (NCT02735707), did show a reduced mortality of additional tocilizumab treatment next to standard of care (RR 0.78; 95% CI 0.63–0.97). In addition, this trial showed that tocilizumab users had a lower risk of disease progression towards mechanical ventilation or death (RR 0.78, 95% CI 0.65–0.94). Clinical worsening or time to improvement were not influenced by tocilizumab administration.
Hydroxychloroquine did not provide mortality benefits for COVID-19 patients (5 RCTs). In fact, 1 RCT on hydroxychloroquine showed that administering this drug could increase mortality rate in this population (RR 1.18; 95% CI 0.90–1.56).
One anakinra RCT was included in the systematic review. No benefits were observed for this drug. The effect of baricitinib (1 RCT) on mortality rate in COVID-19 patients was not significant (RR 0.85; 95% CI 0.40–1.07). Dr Alunno added that, in oxygen-receiving patients, baricitinib plus remdesivir significantly improved mortality rate and shortened the time to recovery. Moreover, the rate of adverse events was not increased by the additional administration of baricitinib.
Dr Alunno concluded that robust evidence on the efficacy of immunomodulatory drugs for the treatment of SARS-CoV-2 infections is limited. The number of investigated outcomes is low and only a few drugs have been studied adequately.
Editor’s note: Since the congress further data has emerged supporting the use of tocilizumab in severe COVID-19 as summarised in a recent meta-analysis [2].
- Alunno A, et al. Immunomodulatory therapies for severe forms of COVID-19: a systematic literature review to inform EULAR points to consider. OP0287, EULAR 2021 Virtual Congress, 2–5 June.
- The WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group. JAMA 2021. DOI: 10.1001/jama.2021.11330.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Faecal microbiota transplantation not effective in active peripheral PsA Next Article
Guselkumab efficacious in PsA patients with inadequate response to TNF inhibition »
« Faecal microbiota transplantation not effective in active peripheral PsA Next Article
Guselkumab efficacious in PsA patients with inadequate response to TNF inhibition »
Table of Contents: EULAR 2021
Featured articles
COVID-19 Update
Rituximab or JAK inhibitors increase the risk of severe COVID-19
Updates on COVID-19 vaccines in patients with rheumatic disease
Immunomodulatory therapies for severe COVID-19: literature update
New Developments in Rheumatoid Arthritis
JAK inhibitors and bDMARDs not associated with increased risk of serious infections in RA
Remote management of RA is a feasible alternative for outpatient follow-up
TOVERA: Ultrasound is a promising biomarker of early treatment response
The risks of polypharmacy in RA
ABBV-3373: A potential new therapeutic agent for RA
JAK inhibitors and bDMARDs show comparable effectiveness
Spondyloarthritis: Progression in Therapies
SELECT-AXIS: 64-week results of upadacitinib in active ankylosing spondylitis
Guselkumab efficacious in PsA patients with inadequate response to TNF inhibition
Faecal microbiota transplantation not effective in active peripheral PsA
Risankizumab meets primary and ranked secondary endpoints in PsA
Prognostic factors for minimal disease activity in early psoriatic arthritis revealed
Imaging in Large-Vessel Vasculitis
PET/CT is a reliable measure of disease activity in LVV, but does not predict future relapses
Ultrasound is useful for disease monitoring in giant cell arteritis
Prevention in Rheumatic Diseases
Air pollution predicts decreased response to biological treatment in rheumatic diseases
Passive smoking associated with an increased risk of RA
Gene-Environment Interaction in Gout
Gene-diet and gene-weight interactions associated with the risk of gout
What Is New in Systemic Lupus Erythematosus
Intensified treatment regimen of anifrolumab for lupus nephritis is promising
Systemic lupus erythematosus: increased risk of severe infection
Juvenile Idiopathic Arthritis and Osteoarthritis
Efficacy and safety of secukinumab in juvenile idiopathic arthritis
Emerging therapies and future treatment directions in osteoarthritis
Related Articles
February 4, 2020
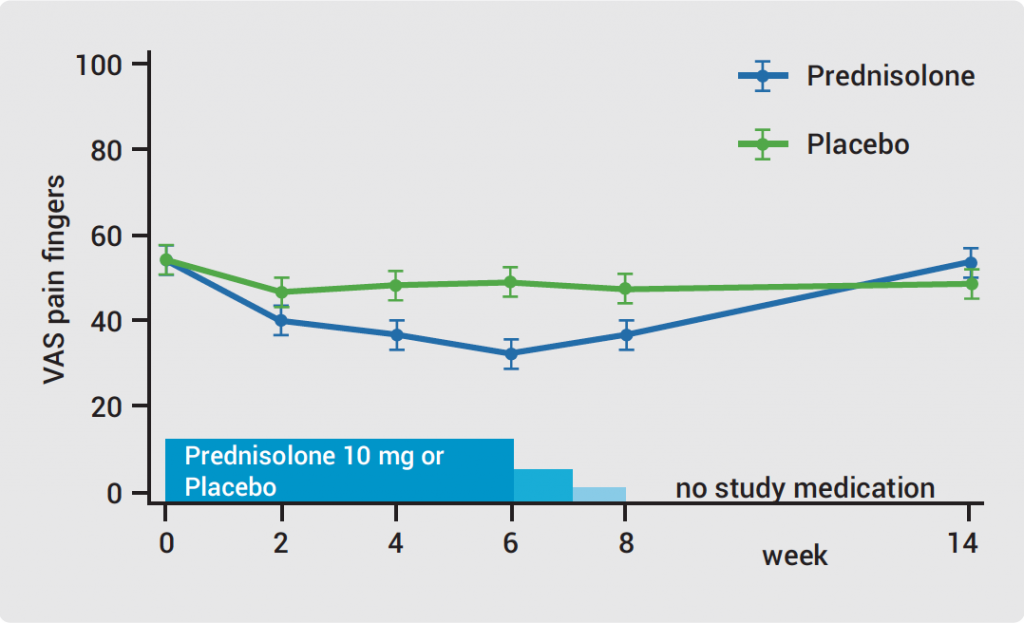
Hand OA: low-dose corticosteroids improve symptoms
November 21, 2024
XG005 relieves OA symptoms in phase 2b study
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

