https://doi.org/10.55788/147579e3
Weight loss and exercise programmes have been shown to be effective in academic, centre-based trials under highly controlled conditions. “However, these interventions have not been rigorously tested in community-based settings,” said Prof. Stephen Messier (Wake Forest University, NC, USA) [1]. Therefore, the primary aim of his study was to determine whether adaptation to a diet and an exercise programme resulted in a statistically significant reduction in pain, compared with a control group.
Thus, 823 patients with OA were randomised and allocated to a diet and exercise group (n=414) or a control group (n=409). The primary outcome was the between-group difference in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) knee pain at the 18-month follow-up. The exercise programme consisted of 15 minutes of walking and 20 minutes of weight training, followed by another 15 minutes of walking. Patients were advised to practice 3 times a week for 18 months. In addition, they received recipes to compose a reduced-calorie diet of their choice with the option to include a nutritional powder to make low-calorie shakes as meal replacements. The control group received nutrition and health education in 5 1-hour face-to-face meetings over the 18 months and informational packets or phone sessions.
The baseline characteristics of both groups were comparable, with a median age of 64 years, a female predominance, and a BMI of 36.7.
Patients in the intervention group achieved a significantly lower WOMAC pain score after 6 and 18 months. At the end of the follow-up period, the WOMAC pain score was reduced by 32% in the intervention group compared with 24% in the control group (P=0.02). Moreover, patients in the intervention group were 20% more likely to attain a 2-point improvement in the WOMAC pain score (considered clinically meaningful) than the control group.
A remarkable success of the diet and exercise programme was noted regarding weight loss: Patients in the intervention group lost 8 kg, which is an 8% weight loss compared with only 2 kg in the control group (P>0.01). The former group also improved WOMAC function: They had a 36% better function compared with 22% in the control group (P<0.001). The intervention also led to a significantly higher mean 6-minute walking distance and a better health-related quality of life.
Prof. Messier concluded that a community-based exercise programme and dietary advice led to a statistically significant albeit modest reduction in pain. In addition, the remarkable weight loss seen in the intervention group can have important additional health benefits.
- Messier S, et al. Effectiveness of Intensive Diet and Exercise on Knee Pain Among Communities with Knee Osteoarthritis, Overweight, and Obesity: The WE-CAN Pragmatic Randomized Clinical Trial. 1675, ACR Convergence 2022, 10–14 November, Philadelphia, USA.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Bruton’s tyrosine kinase inhibition: a novel treatment option for Sjögren’s syndrome? Next Article
Ankylosing spondylitis: Combining biologics with NSAID does not imply reduced radiographic progression »
« Bruton’s tyrosine kinase inhibition: a novel treatment option for Sjögren’s syndrome? Next Article
Ankylosing spondylitis: Combining biologics with NSAID does not imply reduced radiographic progression »
Table of Contents: ACR 2022
Featured articles
Bruton’s tyrosine kinase inhibition: a novel treatment option for Sjögren’s syndrome?
Early treatment: a key to improved outcomes in polyarticular JIA
ACR 2022 Congress Round-Up
Glucocorticoids in rheumatic diseases: Is there a skeletal sparing dose?
Bimekizumab: Robust 1-year results in treating psoriatic arthritis
Stimulation of PD-1: a new concept to treat RA
Denosumab in erosive hand arthritis: Structure repair of interphalangeal joints seems possible
High retention rates after switching between infliximab biosimilars
New analysis assesses the safety of tofacitinib regarding extended MACE
Lack of vaccination results in a higher frequency of pre-term births in pregnant women with rheumatic disease and COVID-19
Ankylosing spondylitis: Combining biologics with NSAID does not imply reduced radiographic progression
Diet and exercise programme: a successful OA strategy in a community-based setting
Bruton’s tyrosine kinase inhibition: a novel treatment option for Sjögren’s syndrome?
A novel risk score helps identify interstitial lung disease in patients with systemic sclerosis
Early treatment: a key to improved outcomes in polyarticular JIA
TYK2 inhibition shows potential as a treatment for SLE
Belimumab efficacious in cutaneous lupus erythematosus
No increased cancer risk in patients with rheumatic diseases and prior malignancy treated with novel therapies
Related Articles
September 4, 2019
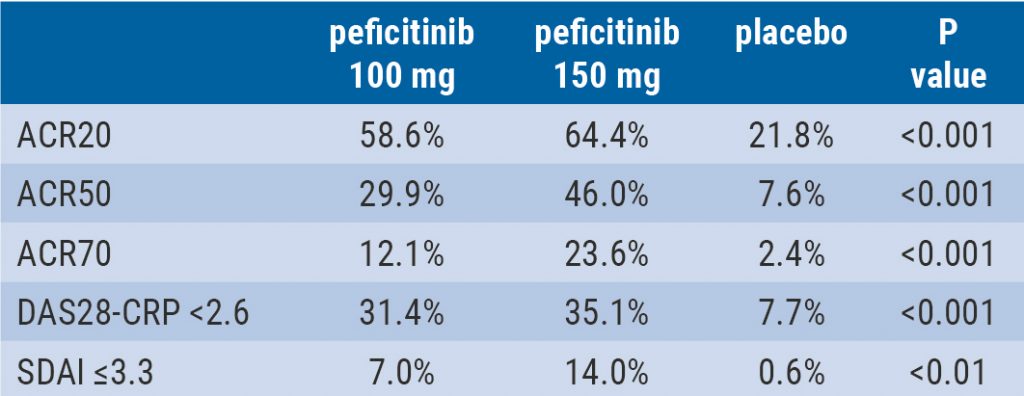
Peficitinib likely efficacious and safe
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

