Type 2 Inflammation
Interview with Prof. Bart Lambrecht, MD, PhD, conducted on 14 November 2019 by Dr Rachel Giles.
Prof. Bart Lambrecht is Professor of Pulmonary Medicine at the University of Ghent, Belgium, and Science Director of the VIB Research Institute-UGent Center for Inflammation Research. His group’s research is focused on unravelling the functions of lung dendritic cells and epithelial cells in asthma and respiratory viral infection.
Prof. Bart Lambrecht: Type 2 inflammation is traditionally associated with diseases like allergic asthma, but there is emerging evidence that type 2 inflammation affecting any organ shares the same pathophysiology, driven by many of the same cell types, such as eosinophils, activated macrophages, and probably even type 2 innate lymphoid cells. For example, fat tissue can either store or burn lipids, and eos
inophils seem to control that metabolic decision. If you have a mouse that genetically lacks eosinophils, a western diet will induce obesity in those mice, demonstrating that eosinophils control energy expenditure and lipid storage [1]. There are other examples as well; there is evidence that eosinophils play a role in the development and involution of the mammary glands during lactation for example [2]. There is also evidence that eosinophils play a role in remodelling of organs after injury [3]. In short, there is more and more evidence that type 2 immunity has a role in normal organismal homeostasis.
How do you think that this shift in metabolism will contribute to the type 2 inflammation itself?
There are long-standing debates about the link between obesity and asthma. One line of thought is that the link between obesity and asthma lies in the fact that you have misdirected immunity. So, your type 2 immunity is involved in asthma, which obstructs its normal regulatory role in metabolism, and consequently, you get an induction of obesity.
Before we can apply this knowledge in the clinic, we will need to wait on the safety data from the BORA trials, a safety trial with 2-year follow-up for people who are on eosinophil-depleting antibodies. So far, no safety signals in humans have been detected with eosinophil depletion but we need to remain vigilant until a longer follow-up has been completed. Therapies blocking type 2 immunity need to be watched for metabolic side effects and one really important question to answer is the role is of type 2 immunity in cancer. There is emerging evidence, mainly from mouse models, that eosinophils can have a protective role against cancer; for example, that eosinophils repress polyp and adenocarcinoma formation in mice heterozygous for the Apc+/- gene [4]. These data are causing a lot of commotion in the field due to the potential implications of risk in humans. However, in humans, the BORA trial has not picked up any increased cancer incidence, although it might be a little bit too premature to completely exclude this risk.
What are the controversies in your field?
From my point of view, one big controversy is that there are huge differences between humans and mice, and we need to be careful not to extrapolate directly between species. It is essential that we only use the murine models to generate hypotheses and understand pathophysiology, but that clinical applications need to be derived from evidence in humans. It seems obvious, but people in our field people use murine data to justify certain clinical choices when this is unsupported by human data.
Another controversy in the field is the heterogeneity of eosinophils. Researchers say that there are “good” eosinophils and “bad” eosinophils, based on the different surface markers. But the controversy is whether any of the type 2-targeting strategies will be able to distinguish the good from the bad eosinophils. Ideally you want to hit the bad eosinophils with a given treatment, and save the good eosinophils, because those are involved in homeostasis and tissue repair. Again, this is derived from data from mice and the data in humans on heterogeneity are very scarce. There is a lot more work to be done in this field.
- Reichman H, et al. Cancer Immunol Res. 2019 Mar;7(3):388-400.
- Gouon-Evans V, et al. Development. 2000 Jun;127(11):2269-82.
- Gieseck RL 3rd, et al. Nat Rev Immunol. 2018 Jan;18(1):62-76.
- Reichman H, et al. Cancer Immunol Res. 2019 Mar;7(3):388-400.
Posted on
Previous Article
« Letter from the Editor Next Article
Interview with ERS president Prof. Tobias Welte »
« Letter from the Editor Next Article
Interview with ERS president Prof. Tobias Welte »
Table of Contents: ERS 2019
Featured articles
Letter from the Editor
Interview with ERS president Prof. Tobias Welte
Holistic View on Asthma
Holistic view on asthma
COPD Management
COPD patients derive clinical benefit from β-blockers
COPD patients harbouring Pseudomonas Aeruginosa face high risk of hospitalisation
One blood eosinophil count is sufficient to guide ICS therapy
Female COPD patients frequently suffer from anxiety and depression
Dual bronchodilation improves ventilation dynamics in COPD patients
Vaping
Vaping impairs innate immune response of the airway
Alternative nicotine delivery products: no help in smoking cessation
Air Pollution
Pregnant women and their offspring: a high-risk group for air pollution
Taxi drivers exposed to highest levels of black carbon pollution
Infectious Respiratory Disease: the Role of Vaccines
Vaccines show multiple positive effects with respect to respiratory health
Pneumococcal vaccines: an effective way to reduce COPD hospitalisations
Interstitial Lung Disease
Antifibrotic therapy slows disease progression in ILD
Reduction of FVC decline in systemic sclerosis-associated ILD
Registry confirms nintedanib efficacy under real-life conditions
Best of the Posters
Fever during immunotherapy for NSCLC associated with shorter PFS
Smart shirt as a device to measure tidal volumes in real-life setting
Exercise with virtual reality beneficial for COPD patients
NSCLC: A new way to evaluate hilar and mediastinal lymph nodes
COPD patients do not benefit from azithromycin therapy longer than a year
Novel Developments in Infectious Disease
Long-term azithromycin decreases exacerbations in primary ciliary dyskinesia
Predicting community-acquired pneumonia outcomes by microRNA testing
Pulmonary Vascular Disease
Balloon pulmonary angioplasty for inoperable chronic thromboembolic pulmonary hypertension
Related Articles
October 26, 2021
Smartphone app improves BP control independent of age, sex, and BMI
November 7, 2018
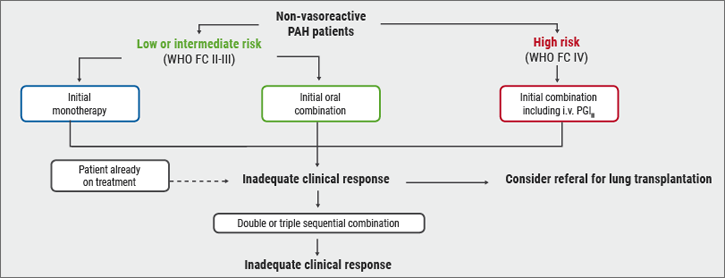
Risk stratification
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

