Longer-term rehabilitation with a duration of 6 weeks is internationally recommended by guidelines as it has shown to improve dyspnoea and exercise tolerance [1,2]. However, in some countries, e.g. Poland and Germany, health insurance generally only approves up to 3 weeks of rehabilitation [1]. Thus, Dr Sebastian Rutkowski (Opole University of Technology, Poland) and his colleagues wanted to find out whether shorter periods of rehabilitation are still able to augment physical performance.
Dr Rutkowski and colleagues also aimed to compare the efficacy of traditional exercise capacity training to a pulmonary rehabilitation programme including non-immersive virtual reality techniques and operated with a gaming console and motion sensor. The 68 included patients were between 50 and 70 years old and suffered from moderate COPD with GOLD stages 2 or 3. Among the exclusion criteria were higher-grade heart failure, insulin-dependent diabetes mellitus, and uncontrolled hypertension. Rehabilitation training took place 5 times a week over 2 weeks either with the virtual reality programme or traditional pulmonary rehabilitation, which included breathing and fitness exercises as well as relaxation training. Primary outcome was defined as improvement in Senior Fitness Test (SFT) performance. Analysis was done with mixed-effects models.
Both groups showed significant ameliorations of the SFT after the 2-week intervention. The members of the virtual reality-group yielded significantly better results in values for arm curl, chair stand, and 6-minutes-walk-test than those in the traditional pulmonary rehabilitation group (P<0.05).
According to Dr Rutkowski, a virtual-reality programme could motivate COPD patients, in particular those with limited activity, to perform regular physical fitness exercises at home.
- Rutkowski S, et al. PA570, ERS 2019, 29 Sept-2 Oct, Madrid, Spain.
- Egan C, et al. Respir Med. 2012;106(12):1671-9.
Posted on
Previous Article
« One blood eosinophil count is sufficient to guide ICS therapy Next Article
COPD patients harbouring Pseudomonas Aeruginosa face high risk of hospitalisation »
« One blood eosinophil count is sufficient to guide ICS therapy Next Article
COPD patients harbouring Pseudomonas Aeruginosa face high risk of hospitalisation »
Table of Contents: ERS 2019
Featured articles
Letter from the Editor
Interview with ERS president Prof. Tobias Welte
Holistic View on Asthma
Holistic view on asthma
COPD Management
COPD patients derive clinical benefit from β-blockers
COPD patients harbouring Pseudomonas Aeruginosa face high risk of hospitalisation
One blood eosinophil count is sufficient to guide ICS therapy
Female COPD patients frequently suffer from anxiety and depression
Dual bronchodilation improves ventilation dynamics in COPD patients
Vaping
Vaping impairs innate immune response of the airway
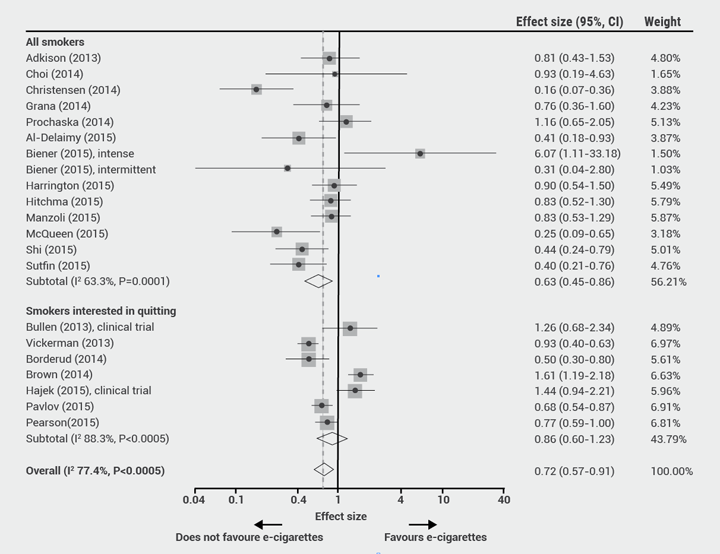
Alternative nicotine delivery products: no help in smoking cessation
Air Pollution
Pregnant women and their offspring: a high-risk group for air pollution
Taxi drivers exposed to highest levels of black carbon pollution
Infectious Respiratory Disease: the Role of Vaccines
Vaccines show multiple positive effects with respect to respiratory health
Pneumococcal vaccines: an effective way to reduce COPD hospitalisations
Interstitial Lung Disease
Antifibrotic therapy slows disease progression in ILD
Reduction of FVC decline in systemic sclerosis-associated ILD
Registry confirms nintedanib efficacy under real-life conditions
Best of the Posters
Fever during immunotherapy for NSCLC associated with shorter PFS
Smart shirt as a device to measure tidal volumes in real-life setting
Exercise with virtual reality beneficial for COPD patients
NSCLC: A new way to evaluate hilar and mediastinal lymph nodes
COPD patients do not benefit from azithromycin therapy longer than a year
Novel Developments in Infectious Disease
Long-term azithromycin decreases exacerbations in primary ciliary dyskinesia
Predicting community-acquired pneumonia outcomes by microRNA testing
Pulmonary Vascular Disease
Balloon pulmonary angioplasty for inoperable chronic thromboembolic pulmonary hypertension
Related Articles
October 22, 2020
Extracorporeal CO2 removal effective in status asthmaticus
November 28, 2019
Alternative nicotine delivery products: no help in smoking cessation
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

