Despite treatment with curative intent, up to 60% of patients with stage I-III NSCLC still experience disease relapse [1]. Impower010 (NCT02486718) is the first randomised phase 3 study to show significant disease-free survival (DFS) improvement with adjuvant cancer immunotherapy (atezolizumab) after adjuvant chemotherapy in patients with early-stage resected NSCLC [2].
Enrolled patients had completely resected stage IB-IIIA NSCLC and ECOG performance status 0–1. A total of 1,280 patients received up to four 21-day cycles of cisplatin-based chemotherapy (plus pemetrexed, docetaxel, gemcitabine, or vinorelbine). Next, 1,005 patients without progression after adjuvant chemotherapy were randomised 1:1 to atezolizumab (1,200 mg every 3 weeks) for 16 cycles or until disease relapse or unacceptable toxicity or to best supportive care (BSC). The primary endpoint was DFS which was hierarchically tested in PD-L1 TC ≥1% (SP263) stage II-IIIA patients (n=476), then in all randomised stage II-IIIA patients (n=882), and then in intention-to-treat patients (n=1,005).
As previously reported, median DFS was significantly improved by atezolizumab in PD-L1 TC ≥1% patients (HR 0.66; P=0.004), and in all randomised patients (HR 0.79; P=0.02), but not in the ITT population (HR 0.81; P=0.04) [2]. Dr Enriqueta Felip (Vall d’Hebron Institute of Oncology, Spain) presented additional results from exploratory analyses in Impower010 [3].
In all randomised stage II-IIIA patients, DFS improvement was seen with increasing PD-L1 expression: TC <1% (n=383) HR 0.97; TC 1–49% (n=247) HR 0.87; and TC ≥50% (n=229) HR 0.43. Among PD-L1 TC ≥1% stage II-IIIA patients (n=676), 73 patients (29%) relapsed in the atezolizumab arm versus 102 patients (45%) in the BSC arm. Sites of relapse in both arms were comparable. Time to relapse appeared to favour the atezolizumab arm over the BSC arm in the PD-L1 TC ≥1% stage II-IIIA patients, with minimal differences seen in the all-randomised and intention-to-treat populations. A higher rate of post-relapse immunotherapy was seen in the BSC arm.
Dr Felip summarised that “in this interim DFS analysis, relapse rate was higher in the BSC arm versus the atezolizumab arm. However, there was no clear difference in pattern of relapse between the arms among patients who relapsed.”
- Vansteenkiste J, et al. Ann Oncol. 2019;30:1244-1253.
- Wakelee HA, et al. J Clin Oncol 39, 2021 (suppl 15; abstr 8500)
- Felip E, et al. Impower010: patterns of relapse and subsequent therapy from a Phase III study of atezolizumab (atezo) vs best supportive care (BSC) after adjuvant chemotherapy (chemo) in stage IB-IIIA non-small cell lung cancer (NSCLC). Abstract LBA9, ESMO Congress 2021, 16–21 September.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Three-year OS follow-up from CASPIAN trial Next Article
Nivolumab/ipilimumab continues to provide survival benefit in unresectable MPM »
« Three-year OS follow-up from CASPIAN trial Next Article
Nivolumab/ipilimumab continues to provide survival benefit in unresectable MPM »
Table of Contents: ESMO 2021
Featured articles
Breast Cancer
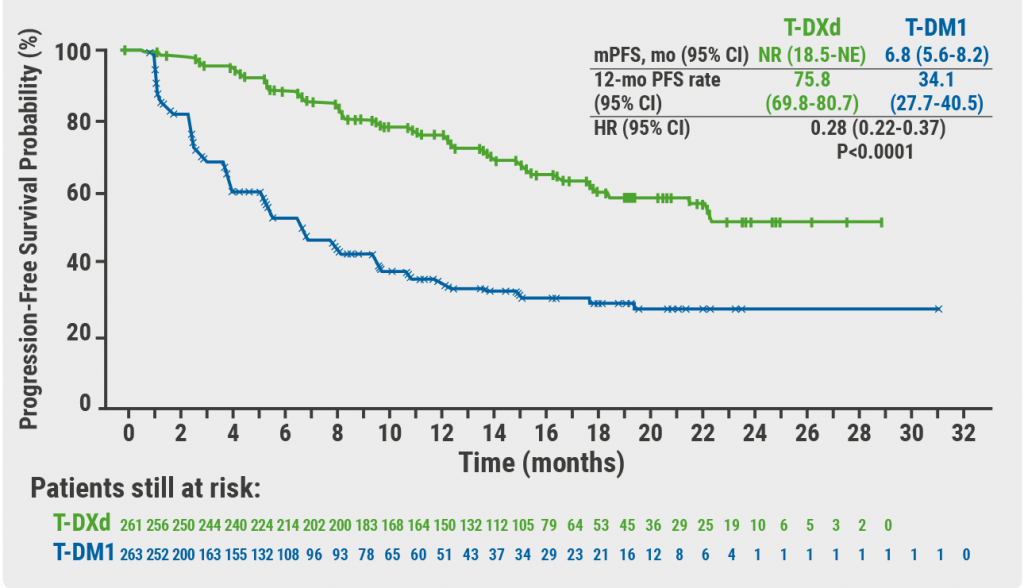
Trastuzumab deruxtecan triples PFS
Novel conjugate meets primary endpoint
Longest survival benefit from first-line CDK4/6 inhibitor
Meta-analysis shows 6-months adjuvant trastuzumab is optimal
Double-positive results for triple-negative metastatic breast cancer
Survival after neoadjuvant therapy with trastuzumab-lapatinib plus chemotherapy
Postmenopausal breast cancer: extended letrozole reduces recurrence
Asian women also benefit from palbociclib plus letrozole
No PEARLs of survival with palbociclib plus endocrine therapy compared with capecitabine, but QoL better
Gastrointestinal Cancer
Neoadjuvant chemotherapy potential alternative to neoadjuvant chemoradiotherapy in LARC
Immune chemo-sensitisation looks promising in microsatellite-stable mCRC
Adagrasib shows promising clinical activity in heavily pretreated KRAS-mutated CRC
Automated detection of microsatellite status on unstained samples in early colon cancer
Consistent benefit of anti-PD-1 therapy for oesophageal and gastric cancer
HIPEC in gastric cancer with peritoneal metastases
ctDNA highly predictive in HER2-positive, advanced gastric or gastro-oesophageal junction cancer
Lung Cancer
Robust anticancer activity of trastuzumab deruxtecan in HER2-mutated NSCLC
Nivolumab/ipilimumab continues to provide survival benefit in unresectable MPM
Adjuvant atezolizumab lowers relapse rate in resected NSCLC
Three-year OS follow-up from CASPIAN trial
TCR clonality predicts pembrolizumab response in NSCLC
Melanoma
Adjuvant immunotherapy reduces risk of disease recurrence in stage II melanoma
IFN-γ signature predicts response to immunotherapy
Updated results of SECOMBIT trial
Combining T-VEC and pembrolizumab does not significantly improve survival in advanced, unresectable melanoma
Durable intracranial responses with nivolumab/ipilimumab
Genitourinary Cancer
TKI drug-free interval strategy not detrimental to conventional continuation strategy in RCC
Modified ipilimumab schedule reduces risk of grade 3/4 adverse events
Optimal neoadjuvant dose ipilimumab/nivolumab in stage III urothelial cancer
Better survival with neoadjuvant dose-dense MVAC regimen in MIBC
PARP inhibitor rechallenge improves PFS in ovarian cancer
Pembrolizumab prolongs survival in persistent, recurrent, or metastatic cervical cancer
Pembrolizumab has durable effect in previously treated MSI-H/dMMR advanced endometrial cancer
HRR mutational status is prognostic and predictive biomarker olaparib activity
Haematological Cancer
Mutational analyses are predictive in malignant lymphomas
Low numbers of M2 macrophages in tumour microenvironment associated with superior response to immunotherapy in Hodgkin lymphoma
COVID-19
Adequate response to SARS-CoV-2 vaccine in cancer patients
Cancer patients more likely to die from COVID-19 when hospital admittance is required
Third global survey of the ESMO Resilience Task Force
High COVID-19 mortality in Swiss cancer patients
Basic Science & Translational Research
Neutrophils negatively correlate with response to anti-PD-1 monotherapy in dMMR tumours
Tetraspecific ANKETs harnesses innate immunity in cancer therapies
Early ctDNA reduction in metastatic uveal melanoma correlates better with OS than RECIST response
Gut microbiota as a potential predictive biomarker
Related Articles
November 19, 2021
Trastuzumab deruxtecan triples PFS
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

