HER2-positive early-stage breast cancer is a particularly aggressive, and neoadjuvant chemotherapy plus HER2-targeted therapy is the standard of care. Despite its efficacy, patients remain at increased risk of recurrence, mortality, and taxane-related toxicity, making it critical to optimize HER2-targeted treatment and determine who might benefit the most.
“In 2005, we were lucky to have one HER2-targeted therapy to combine with chemo[therapy] for patients with HER2-positive early-stage disease, and in 2020 we have four HER2-targeted agents available. However, clearly not everyone needs trastuzumab and chemotherapy,” discussant Sara A. Hurvitz, MD, of the University of California, Los Angeles, said. “We find ourselves in a bit of a Goldilocks conundrum, where we need to choose the therapy that is ‘just right’ for our patients.”
In an effort to help achieve this, the phase III KAITLIN trial compared survival and tolerability outcomes from the use of T-DM1 with pertuzumab versus standard of care.
Women with HER2-positive early-stage breast cancer received three to four cycles of adjuvant anthracycline (doxorubicin or epirubicin) and were then randomly assigned to either up to 18 cycles of T-DM1 (3.6 mg/kg) plus pertuzumab (420 mg; KP arm; 928 patients), or up to 18 cycles of trastuzumab (6 mg/kg) plus pertuzumab (420 mg) and three to four cycles of taxanes (THP arm; 918 patients). Primary endpoints were iDFS in the node-positive and intention-to-treat populations. Secondary endpoints were overall survival in both populations, disease-free survival, distant recurrence–free interval, safety, and patient-reported health status/quality of life.
There were no differences in iDFS between treatments in the node-positive and intention-to-treat groups. This was consistent across several subgroups (e.g., node status, central hormone receptor status, type of anthracycline, and geographic region). There was no clinically relevant subgroup that favored one study arm over the other.
“However, I think it’s noteworthy to look at the excellent 3-year iDFS in this high-risk population,” Dr. Harbeck said. “About 30% [of all patients] had more than four involved lymph nodes, but we see here about 93% iDFS in both [treatment] arms.”
The KP and THP regimens both demonstrated acceptable safety profiles, with comparable rates of grade 3 or greater adverse events (52% vs. 55%) and serious adverse events (21% vs. 23%). However, withdrawal from T-DM1 or trastuzumab because of adverse events was higher among patients receiving KP than those receiving THP (27% vs. 4%).
Finally, there was a lower risk of deterioration of patient-reported health status/quality of life in the KP group.
Dr. Hurvitz noted that re-examining KP versus THP but using a noninferiority study design would be beneficial and might have resulted in the primary endpoint being met. Not testing T-DM1 alone also represented a missed opportunity, she said.
However, Dr. Hurvitz emphasized that, despite failing to detect superiority among treatments, iDFS outcomes from the KAITLIN trial support those from the KRISTINE trial, which also examined T-DM1 plus pertuzumab, and improve upon survival outcomes from other node-positive/HER2-positive trials (Table) [2].
Table. Outcomes for LN+ HER+ disease with HER2-targeted adjuvant therapy from modern studies

Abbreviations: DFS, disease-free survival; LN, lymph node.
- Harbeck N, et al. ASCO Virtual Meeting, 29-31 May 2020, AbstractAbbreviations: DFS, disease-free survival; LN, lymph node.
- Hurvitz SA, et al. Lancet Oncol. 2018;19(1):115‐126.
- von Minckwitz G, et al. N Engl J Med. 2017;377(2):122‐131.
- Perez EA, et al. J Clin Oncol. 2011;29(25):3366‐3373.
- Slamon D, et al. N Engl J Med. 2011;365(14):1273‐1283.
Posted on
Previous Article
« Maintenance olaparib improves OS in relapsed ovarian cancer with BRCA1/2 mutation Next Article
Advanced breast cancer: locoregional therapy does not improve OS »
« Maintenance olaparib improves OS in relapsed ovarian cancer with BRCA1/2 mutation Next Article
Advanced breast cancer: locoregional therapy does not improve OS »
Table of Contents: ASCO 2020
Featured articles
COVID-19 & Telemedicine
COVID-19 and Cancer Consortium Registry: initial results
Oncology hospital-at-home model reduces hospitalizations, emergency department visits, and costs
Nurse-led telephone triage system reduces hospitalizations, helps patients manage symptoms at home
Melanoma
Adjuvant pembrolizumab: durable RFS for stage III melanoma
Adjuvant pembrolizumab: durable RFS for stage III melanoma
Pembrolizumab plus low-dose ipilimumab well tolerated after progression on PD1 antibody therapy
Toripalimab plus axitinib effective in metastatic mucosal melanoma
Breast & Ovarian Cancer
Advanced breast cancer: locoregional therapy does not improve OS
T-DM1 does not improve safety or efficacy in HER-2 positive early breast cancer; favorable iDFS reported
Maintenance olaparib improves OS in relapsed ovarian cancer with BRCA1/2 mutation
Combination pembrolizumab/chemo improves PFS in metastatic TNBC
Effect of veliparib with or without cisplatin in breast cancer: results of SWOG S1416
PHOEBE, a phase 3 trial comparing pyrotinib and lapatinib in HER2-positive metastatic breast cancer
BYLieve demonstrates efficacy of PIK3CA-directed treatment post CDK4/6-ihibition
Strategies emerge for chemotherapy de-escalation in HER2-positive breast cancer
Multiple Myeloma
Carfilzomib: no PFS benefit for multiple myeloma
Lung Cancer
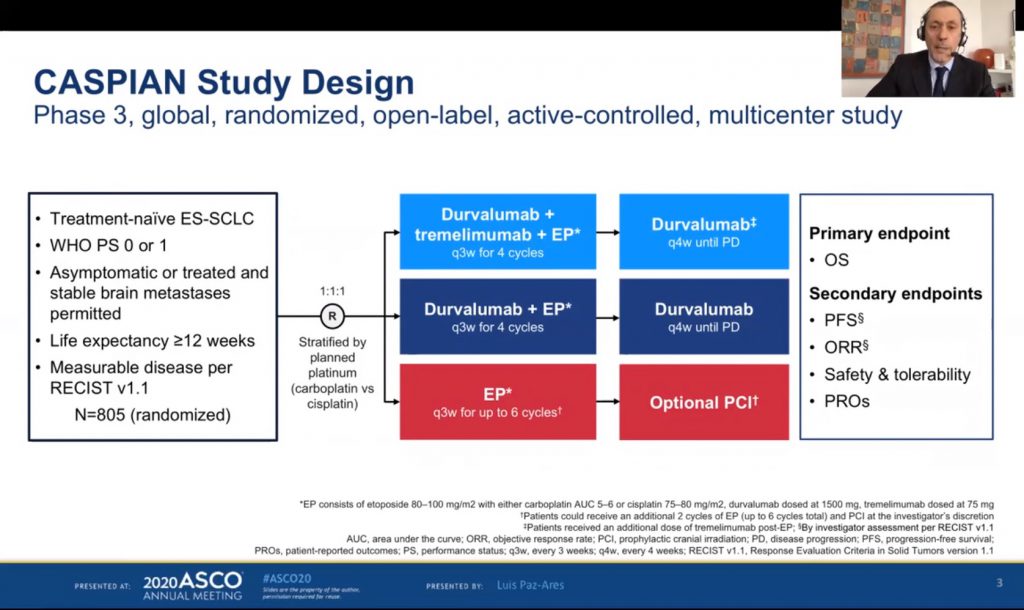
ES-SCLC: tremelimumab + durvalumab + chemotherapy misses endpoint
Adjuvant osimertinib in NSCLC: practice changing ADAURA trial
ES-SCLC: pembrolizumab KEYNOTE-604 data
Second-line gemcitabine plus ramucirumab significantly improves overall survival
Tiragolumab and atezolizumab: ORR in NSCLC
MET-amplified advanced NSCLC responds well to MET inhibitor capmatinib
Genitourinary Cancer
Urothelial cancer: avelumab works as maintenance therapy
ARAMIS final OS and nmCRPC safety outcomes
Final survival results from phase 3 SPARTAN trial
Novel drug for kidney cancers/VHL patients
Primary analysis from IMvigor010, adjuvant atezolizumab in high risk muscle-invasive urothelial carcinoma
First randomised trial of Lu-PSMA in mCRPC progressing after docetaxel
Gastrointestinal Cancer
HER2-expressing metastatic colorectal cancer: trastuzumab deruxtecan
REGOMUNE: a phase 2 study combining regorafenib and avelumab
Cardiotoxicity: consider switching to S-1
Perioperative chemotherapy for resectable pancreatic ductal adenocarcinoma
Real-world data of sequential sorafenib followed by regorafenib in unresectable HCC
Paediatric Cancer
Sustained improvements in quality of life with larotrectinib
Promising first immunotherapy trial in placental trophoblastic tumours
Precision medicine for poor-prognosis paediatric patients
Related Articles
August 28, 2020
Carfilzomib: no PFS benefit for multiple myeloma

September 8, 2020
ES-SCLC: tremelimumab + durvalumab + chemotherapy misses endpoint
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

