https://doi.org/10.55788/e518c218
In recent years, the rate of HA-VTE has been increasing in the paediatric population [1]. Dr Julie Jaffray (Rady Children’s Hospital-San Diego, CA, USA) explained: “We know that critical illness and central venous catheters are the most important risk factors, with an incidence of HA-VTE of up to 18% in patients who have both these risk factors [2].” Various RAMs for critically ill children have been distilled from single-centre studies, but have not been externally validated. The current study aimed to prospectively validate the HA-VTE RAM, a retrospectively derived multi-institutional RAM for critically ill children [3], externally in an independent cohort via the CHAT consortium [4].
Participants between 0 and 21 years of age who were admitted to a paediatric IC unit were randomly selected and enrolled in the study. In total, 3,139 participants were included in the validation analysis [4].
The incidence of HA-VTE was 2.1% in the study population. The receiver operator characteristic (ROC) of the model was 0.81 (95% CI 0.75–0.86). Factors contributing significantly to an increased risk of HA-VTE were: immobility within 24 hours of admission (OR 1.99; 95% CI 1.16–3.44; P=0.013), past medical history of cancer (OR 3.09; 95% CI 1.42–6.72; P=0.004), hospitalisation up to 30 days before the current hospitalisation (OR 1.99; 95% CI 1.14–3.47; P=0.016), mechanical ventilation within 24 hours of admission (OR 1.91; 95% CI 1.07–3.40; P=0.028), and placement of a central venous catheter within 30 days before or within 24 hours of admission (OR 4.19; 95% CI 2.38–7.38; P<0.001).
“The assessed HA-VTE RAM helps us to understand which subset of critically ill children may benefit from thromboprophylaxis measures without increasing bleeding risk,” concluded Dr Jaffray.
- O’Brien SH, et al. Pediatrics. 2022;149(3):e2021054649.
- Faustino EVS, et al. J Pediatr. 2013;162(2):387-391.
- Jaffray J, et al. Pediatr Crit Care Med. 2022;23(1):e1-e9
- Jaffray J, et al. Multicenter study of a risk assessment model for critically ill children at high-risk for hospital-acquired venous thromboembolism. Abstract 809, 65th ASH Annual Meeting, 9–12 December 2023, San Diego, CA, USA.
Copyright ©2024 Medicom Medical Publishers
Posted on
Previous Article
« Axatilimab may present a new therapeutic strategy in chronic GvHD Next Article
Favourable QoL and bleeding outcomes for rilzabrutinib in ITP »
« Axatilimab may present a new therapeutic strategy in chronic GvHD Next Article
Favourable QoL and bleeding outcomes for rilzabrutinib in ITP »
Table of Contents: ASH 2023
Featured articles
Meet the Trialist: Prof. Jeff Sharman on ELEVATE-TN
Leukaemia
FLT3-ITD-specific MRD assessment useful for clinical management of AML
MRD status rather than FLT3-ITD co-mutation is linked to the benefit of CR1-allo in NPM1-mutated AML
Promising results for quizartinib, venetoclax, and decitabine in FLT3-ITD mutated AML
AUGMENT-101: Excellent results for revumenib in R/R KMT2Ar leukaemia
Blinatumomab reduces toxicity in the consolidation phase in paediatric high-risk B-cell ALL
Promising results for olverembatinib in combination with venetoclax for Ph+ ALL
Undetectable MRD on maintenance venetoclax, acalabrutinib, and obinutuzumab in the majority of R/R CLL participants
Lymphoma
Is allogeneic stem cell transplantation a solid option in R/R LBCL or R/R T-cell lymphoma?
Encouraging results for the addition of acalabrutinib to lenalidomide and rituximab in follicular lymphoma
Can ibrutinib ameliorate outcomes in R/R ABC-DLBCL undergoing autoSCT?
Primary phase 2 efficacy and safety results of M-Pola in relapsed/refractory LBCL
SYMPATICO: Ibrutinib plus venetoclax boosts PFS in R/R mantle cell lymphoma
Multiple Myeloma
KdD outperforms Kd in R/R MM also in participants with poor renal function
IsKia: Novel treatment regimen for MM delivers high MRD-negativity rates
Novel standard-of-care in newly diagnosed MM
Myeloproliferative Neoplasms
TRANSFORM-1: High spleen volume reduction rates for navitoclax plus ruxolitinib in myelofibrosis
Momelotinib beats controls regarding transfusion outcomes in myelofibrosis
DALIAH: Peginterferon-α head-to-head against hydroxyurea in MPN
Non-Malignant Haematology
Long-term efficacy and safety of iptacopan in PNH with anaemia
ADVANCE IV: Swift responses on efgartigimod in ITP
Favourable QoL and bleeding outcomes for rilzabrutinib in ITP
Novel risk assessment model acts on increasing hospital-acquired venous thromboembolism rates among children
Miscellaneous Topics
Axatilimab may present a new therapeutic strategy in chronic GvHD
Pomalidomide may become the first approved therapy for hereditary haemorrhagic telangiectasia
Ancestry-specific study into CH delivers new leads
Featured Interviews
Interview: Sandwich treatment model shows promise for mantle cell lymphoma
Meet the Trialist: Prof. Jeff Sharman on ELEVATE-TN
Related Articles
September 9, 2020
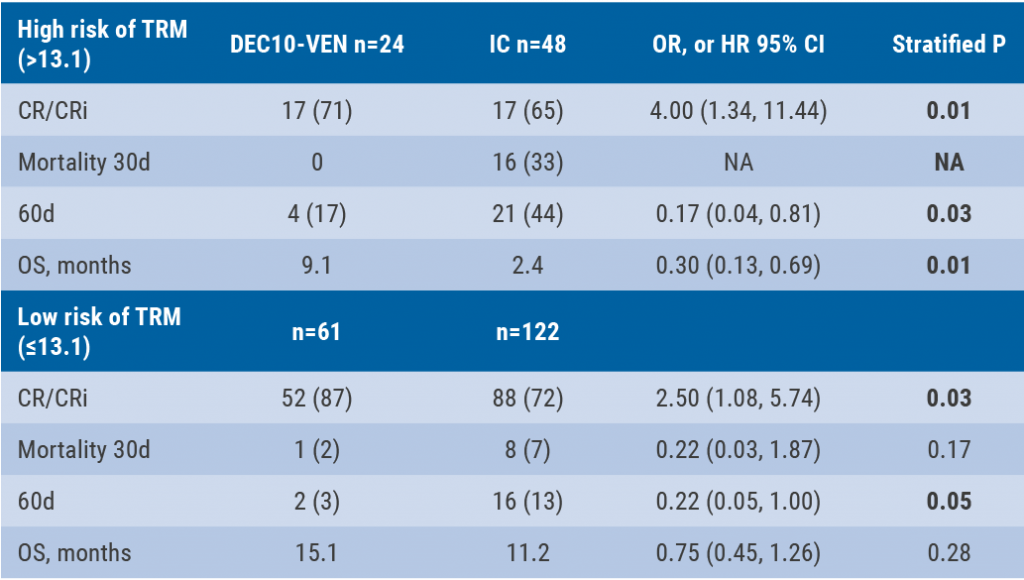
DEC10-VEN superior to intensive chemotherapy in high-risk AML
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

