CD19 CAR T cells have revolutionised the treatment of relapsed/refractory (R/R) LBCL, resulting in durable and complete responses in approximately 40-50% of patients [2]. “We wanted to focus on patients who do not obtain durable and complete responses, because the outcome of these patients is really poor, with a median overall survival (OS) of <200 days [3],” Dr Majzner explained [1]. “Because CAR T cells are able to induce long-term remission in patients, we feel that if we can get the initial response rate up and find the mechanisms of resistance and engineer around that, we can cure more patients.” Besides a loss or decrease in CD19 expression, no studies have identified tumour-specific factors driving resistance to CAR T cells in LBCL. Mutations in and loss of expression of CD58 have been described in approximately 20% of LBCL cases. CD58 loss or mutation has been linked to immune resistance in LBCL [1].
Dr Majzner and his team evaluated CD58 status in 51 R/R LBCL patients with axicabtagene ciloleucel (axi-cel) through immunohistochemistry on tumour biopsy samples and/or deep sequencing of circulating tumour DNA; 24% of these patients had a CD58 aberration. Progression-free survival (PFS) was significantly decreased in patients with a CD58 aberration (median 3 months vs not reached for CD58 intact; P<0.0001). Only 1 patient with a CD58 alteration achieved a durable, complete response to axi-cel and the remaining 11 patients progressed, most commonly after a period of initial response [1].
To overcome CD58 loss in LBCL, the researchers generated second- and third-generation CAR T-cell constructs. While these constructs demonstrated increased potency against CD58 knock-out cells in vitro, they were unable to ultimately overcome CD58 loss in vivo. However, when CARs were co-expressed with an additional CD2 receptor, they mediated significant anti-tumour activity in vivo, overcoming CD58 knockout in tumour cells [1].
These data provide rationale for investigating CD58 status for patients receiving CAR-based therapeutics. “We have now been able to engineer CARs to integrate CD58-CD2 signalling in a specific manner to overcome CD58 loss and re-establish CAR efficacy, independent of CD58 on the tumour cell line,” Dr Majzner concluded. “We think that this will end up in other malignancies as well, because CD58 mutations are common in other cancers, including myeloma and Hodgkin lymphoma, and are likely able to mediate resistance to other CARs and immunotherapeutics.”
- Majzner RG, et al. CD58 Aberrations Limit Durable Responses to CD19 CAR in Large B Cell Lymphoma Patients Treated with Axicabtagene Ciloleucel but Can be Overcome through Novel CAR Engineering. 62nd ASH Annual Meeting, 5-8 December 2020. Abstract 556.
- Neelapu SS, et al. N Engl J Med. 2017;377:2531-44.
- Spiegel JY, et al. Blood. 2020;blood.2020006245.
Posted on
Previous Article
« “Strongly consider an SGLT2-inhibitor in most T2DM patients” Next Article
Deep and durable responses with ide-cel in RRMM »
« “Strongly consider an SGLT2-inhibitor in most T2DM patients” Next Article
Deep and durable responses with ide-cel in RRMM »
Table of Contents: ASH 2020
Featured articles
COVID-19
More complicated course of COVID-19 in leukaemia patients
Older age and imatinib treatment associated with COVID-19 mortality in CML
Allogeneic SARS-CoV-2-specific T cells to treat COVID-19
More severe COVID-19 outcomes for patients with haematologic malignancies
Acute Lymphoblastic Leukaemia
Improved outcomes, but still substantial part experiences relapses
Strong correlation between peripheral blood and bone marrow NGS MRD
Encouraging outcomes after autoHCT in patients with ALL
Acute Myeloid Leukaemia
Prognostic validity of AML composite model in predicting mortality
Venetoclax plus hypomethylating agents in favourable-risk AML
Encouraging clinical activity of decitabine plus ipilimumab in R/R or secondary MDS/AML
AML patients with specific mutations are unlikely to achieve MRD
Comparable outcomes with gilteritinib or quizartinib in R/R AML
First-in-class macrophage immune checkpoint inhibitor in AML
Bispecific DART® as salvage therapy for primary induction failure and early relapse
Gilteritinib in R/R AML patients priorly treated with midostaurin or sorafenib
Addition of venetoclax provides an effective, lower-intensity regimen
Chronic Leukaemia
Bosutinib effective and well tolerated in newly diagnosed CP-CML
Efficacy and safety of ponatinib in patients with CP-CML who failed second-generation TKIs
First-in-class STAMP inhibitor versus bosutinib in resistant or intolerant CML
PFS and ORR benefits of first-line ibrutinib-based treatment in CLL
Multiple Myeloma
Validation of MY-RADS response assessment category criteria
High symptom burden in transplant-ineligible patients with newly diagnosed MM
Added value of ixazomib to lenalidomide plus dexamethasone in transplant-ineligible newly diagnosed MM
Survival of transplant-eligible newly diagnosed MM in FORTE trial
Better survival with upfront autoSCT versus bortezomib-based intensification
Subcutaneous daratumumab plus pomalidomide and dexamethasone in R/R MM
Melflufen well tolerated with encouraging activity in heavily pretreated R/R MM
Initial data of FcRH5/CD3 T-cell-engaging bispecific antibody
Lymphoma
CD58 aberrations limit durable responses to CD19 CAR T-cell therapy
Anti-CD19 CAR T-cell therapy in relapsed/refractory indolent NHL
Myeloproliferative Neoplasms
MPN disease burden, quality of life, and treatment patterns
Interventions in JAK/STAT signalling pathway
Novel, orally available inhibitor of BCL-XL/BCL-2
New insights into genetics of MPN
Immune Thrombocytopenia
Mycophenolate efficacious and tolerable, even in elderly patients
First-in-class antibody sutimlimab selectively inhibits classical complement pathway
BTK inhibition provides clinically active and durable platelet response
Haemophilia, Sickle Cell Disease, Thalassaemia
First results from gene therapy trial in haemophilia B
Impact of haemophilia on children and their caregivers
Promising CRISPR gene editing results in β-thalassaemia and sickle cell disease
Erythroid maturation agent in patients with β-thalassaemia requiring regular RBC transfusions
Related Articles
February 18, 2021
More complicated course of COVID-19 in leukaemia patients
February 18, 2021
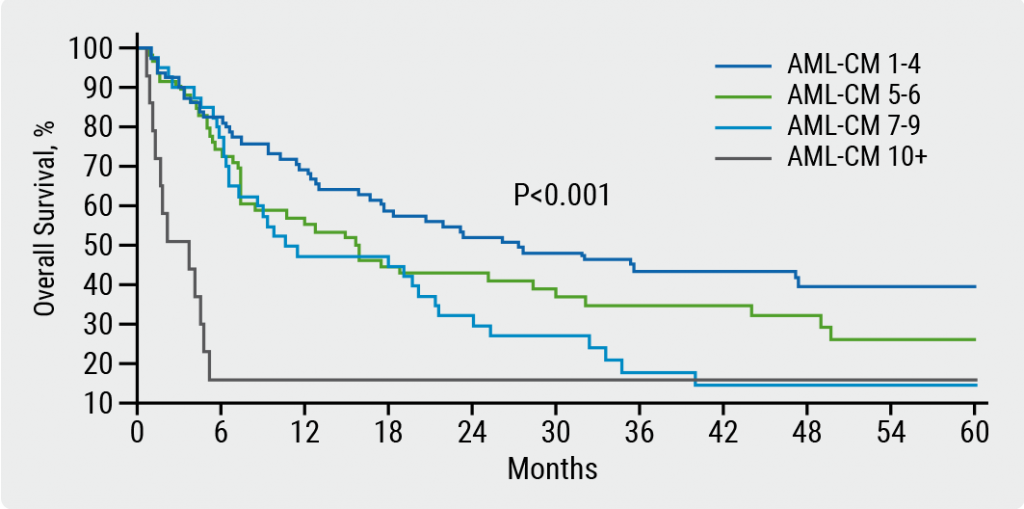
Prognostic validity of AML composite model in predicting mortality
February 18, 2021
Improved outcomes, but still substantial part experiences relapses
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

