Psoriasis is a Th1 and/or Th17 cell-mediated autoimmune disease affecting the skin of genetically predisposed individuals. It has been 15 years since a key innate immune pathway was uncovered for triggering psoriasis [1]. In the early (acute) phase, plasmacytoid dendritic cells (pDCs) accumulate in the skin of psoriasis patients and become activated, for example by mechanical stimulation of the skin to produce interferon (IFN)α. Through the production of IFNα, pDCs drive the activation and expansion of autoimmune T cells in pre-psoriatic skin, leading to the development of psoriasis. In contrast, IFNα does not play a role in the chronic phase of the disease. Accordingly, therapy with MEDI-545, a fully human anti-IFNα monoclonal antibody, failed to show a therapeutic effect in established plaque psoriasis [2].
“Tumour necrosis factor (TNF) blockers have been the gold standard for 10 years in the therapy of plaque psoriasis,” Prof. Curdin Conrad (Lausanne University Hospital, Switzerland) said [3]. A well-known side effect of anti-TNF therapy is psoriasiform eruptions, which resemble classical psoriasis but are immunologically distinct. Numerous cases have been published in the literature. “About 2–5% of patients receiving anti-TNF treatment develop paradoxical psoriasis independent of underlying disease,” Prof. Conrad said. The pathogenesis of this phenomenon is unknown. Paradoxical psoriasis is a class effect of all anti-TNFs. Prof. Conrad pointed out that this phenomenon is selective for anti-TNF and a side effect of TNF-blocker, not de novo psoriasis. “If you switch patients to another class of drugs, psoriasis disappears,” Prof. Conrad explained. In contrast to classic plaque psoriasis, only skin lesions of patients with paradoxical psoriasis show overexpression of both IFNα2 and IFN-ß1 [4]. Other characteristics only seen in paradoxical psoriasis are a dermal accumulation of pDCs and reduced T-cell numbers. Anti-TNF treatment prolongs type I interferon production by pDCs through inhibition of their maturation. The resulting type I interferon overexpression is responsible for the skin phenotype of paradoxical psoriasis, which, unlike classical psoriasis, is independent of T cells [4].
Paradoxical psoriasis: a type I interferon-driven innate inflammation
Thus, paradoxical psoriasis represents an ongoing, overactive innate inflammatory process, driven by pDC-derived type I interferon that does not lead to T-cell autoimmunity [4]. “Based on this, we proposed the so-called Yin and Yang of TNF and IFNα, where those 2 cytokines represent opposing vectors (TNF/IFNα),” Prof. Conrad said. TNF-inhibitors can dysregulate this balance and thus induce an IFN-driven inflammation. “Although the clinical picture is very similar, the pathogenesis of classical psoriasis and paradoxical psoriasis is completely opposing. One is driven by TNF, is a T-cell mediated disease and therefore shows relapses, while the other is induced by the blockade of TNF, is T-cell independent, and therefore does not show any relapses and represents an ongoing IFNα-driven innate inflammation,” Prof. Conrad explained.
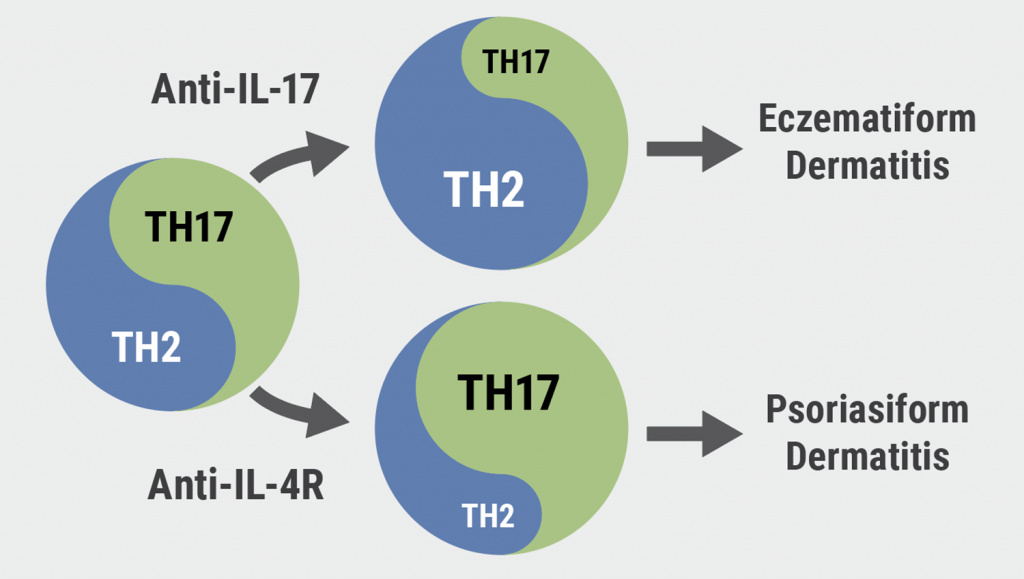
“Depending on the genetic background, you could get other side effects than paradoxical psoriasis. Something that gets activated through interferon is B cells, so one could get an induction of autoimmune antibodies or lupus or even an induction of anti-drug antibodies – all linked to the same pathway,” Prof. Conrad explained. So, is this Ying-Yang concept true for TNF/IFNα only, or is it a general concept in immunology that 2 opposing vectors or 2 pathways control each other? Indeed, there is another example: Biologics targeting IL-17A can induce eczema and pruritus in patients with plaque psoriasis. Eczematous skin lesions develop despite initial response to anti-IL-17A therapy. Eczematous manifestations are noticed in 5–6% of anti-IL17A-treated patients and show no association with atopy. “Typically, these lesions are seen after a good resolution of the underlying psoriasis,” according to Prof. Conrad. In patients with eczema following anti-IL-17A treatment, he found a complete switch from Th17 to Th2 signature typical for atopic dermatitis. “Based on this, we also propose to see the Th17 and Th2 pathways as a Yin and Yang” (see Figure). Blockade of Th17 can lead to a switch to Th2 disease like atopic dermatitis. Vice versa, psoriasiform skin lesions developed despite a response of eczematous lesion to anti-IL-4R, 3 months after the start of dupilumab [5]. “These experiences suggest that Th2/Th17 pathways control each other, and the Yin-Yang between 2 opposing vectors seems to be a general concept in immunology. At least 2 could be described, between TNF and type I interferon and between Th17 and Th2. “Therefore, selective targeting of an inflammatory pathway may displace the inflammatory balance,” Prof. Conrad concluded.
Figure: The Yin-Yang of Th2/Th17 [1]
- Nestle FO, et al. J Exp Med 2005;202:135–143.
- Bissonnette R, et al. J Am Acad Dermatol 2010;62:427–436.
- Conrad C. Paradoxical reactions to biologics: mechanisms, features and management. Psoriasis from Gene to Clinic 2021, 9–11 December.
- Conrad C, et al. Nat Commun 2018;9:25.
- Ferrucci S, et al. Clin Exp Dermatol 2020;45:625–626.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Explaining arthropathy development through IL-4 and IL-13 blockade Next Article
High treatment success with ixekizumab in patients with psoriasis and diabetes »
« Explaining arthropathy development through IL-4 and IL-13 blockade Next Article
High treatment success with ixekizumab in patients with psoriasis and diabetes »
Table of Contents: PFGC 2021
Featured articles
Letter from the Editor
Guselkumab shows highest drug survival among systemic treatments
Genes in Psoriasis and Psoriatic Arthritis
HLA-C*06:02-positive patients on ustekinumab show higher drug survival in a real-world scenario
Protective factors identified against anti-drug antibody formation to adalimumab in psoriasis
Comorbidity in Psoriasis
Psoriasis associated with a higher cancer risk
Comorbidity and clinical features of psoriasis vary according to HLA-C*06:02 status
Psoriasis patients with cardiovascular comorbidity characterised by high systemic inflammation
Psoriasis Therapy: New Findings
Inhibition of heat shock protein: A novel way to treat psoriasis?
Guselkumab shows highest drug survival among systemic treatments
Tapering biologics: No alarming signs of increased anti-drug antibodies
Intermediate monocytes are possible predictors of response to secukinumab
Gut microbiota of psoriasis patients: less diverse and reduced functionality
COVID-19: What's New
DLQI scores underestimated during lockdowns?
TNF blockers likely beneficial for psoriatic patients with COVID-19
Patients on immunomodulators need 2 COVID-19 vaccinations before seroconversion
Paradoxical Reactions to Biologics
The Yin and Yang of opposing vectors: an explanation for side effects of biologics
Explaining arthropathy development through IL-4 and IL-13 blockade
Best of the Posters
Potential biomarker discovered for treatment response to ustekinumab
TNF inhibitor for immune-mediated inflammatory disease doubles the risk of paradoxical psoriasis
Secukinumab also tolerable in paediatric psoriasis patients
High treatment success with ixekizumab in patients with psoriasis and diabetes
Related Articles
July 17, 2024
Managing obesity and fibromyalgia in psoriatic disease
September 28, 2021
Could steroid treatment speed recovery from infliximab-induced liver injury?
November 18, 2021
Grand debate: Is psoriasis a systemic or skin-only disease?
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

