Some patients with immune-mediated inflammatory disease develop paradoxical induction or worsening of psoriasis during treatment with TNFα inhibitors. As this side effect is poorly understood, a Danish cohort study explored the risk of new-onset psoriasis during treatment with a TNF inhibitor compared with the risk during treatment with non-biologic conventional treatment [1]. Dr Nikolai Loft (Copenhagen University Hospital, Denmark) and colleagues evaluated the risk of developing any type of psoriasis, non-pustular and pustular psoriasis. Data was derived from the Danish national registries, which includes all patients with inflammatory bowel disease (IBD) and/or rheumatoid arthritis (RA) who received either conventional therapy or TNF inhibitor treatment between 1995 and 2018.
The analysis included 20,910 patients treated with TNF inhibitors, of whom 108,024 patients were treated conventionally, and 4,909 patients were treated with non-TNF inhibitor biologics. During the follow-up period, 1,471 (1.4%) patients developed psoriasis. Most patients (n=1,332) suffered from non-pustular psoriasis, another 127 from psoriasis pustulosis palmoplantaris, and 12 from generalised pustular psoriasis.
The relative risk of developing non-pustular psoriasis during treatment with a TNF inhibitor was 2.12 times higher than with conventional treatment. An even higher risk of TNF inhibitor intake was associated with developing pustular psoriasis (HR 6.5). When the risk of TNF inhibitor use was compared with the risk of non-TNF biologics, TNF inhibitor use was associated with an HR of 1.85 for non-pustular and 3.11 for pustular psoriasis. Based on this data, the researchers calculated that exposure to TNF inhibitors for 241 patient-years is needed for 1 additional patient with any type of TNF inhibitor-induced psoriasis. Although non-pustular types for psoriasis constituted the most events, pustular types of psoriasis had the highest relative risk. The researchers emphasised that practitioners who treat patients with immune-mediated inflammatory disease should be aware of the risk of TNF inhibitor-induced psoriasis.
- Thein D, et al. Risk of anti-TNF-induced psoriasis in patients with immune‐mediated inflammatory diseases – a Danish nationwide cohort study. P27, Psoriasis from Gene to Clinic 2021, 9–11 December.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Secukinumab also tolerable in paediatric psoriasis patients Next Article
Potential biomarker discovered for treatment response to ustekinumab »
« Secukinumab also tolerable in paediatric psoriasis patients Next Article
Potential biomarker discovered for treatment response to ustekinumab »
Table of Contents: PFGC 2021
Featured articles
Letter from the Editor
Guselkumab shows highest drug survival among systemic treatments
Genes in Psoriasis and Psoriatic Arthritis
HLA-C*06:02-positive patients on ustekinumab show higher drug survival in a real-world scenario
Protective factors identified against anti-drug antibody formation to adalimumab in psoriasis
Comorbidity in Psoriasis
Psoriasis associated with a higher cancer risk
Comorbidity and clinical features of psoriasis vary according to HLA-C*06:02 status
Psoriasis patients with cardiovascular comorbidity characterised by high systemic inflammation
Psoriasis Therapy: New Findings
Inhibition of heat shock protein: A novel way to treat psoriasis?
Guselkumab shows highest drug survival among systemic treatments
Tapering biologics: No alarming signs of increased anti-drug antibodies
Intermediate monocytes are possible predictors of response to secukinumab
Gut microbiota of psoriasis patients: less diverse and reduced functionality
COVID-19: What's New
DLQI scores underestimated during lockdowns?
TNF blockers likely beneficial for psoriatic patients with COVID-19
Patients on immunomodulators need 2 COVID-19 vaccinations before seroconversion
Paradoxical Reactions to Biologics
The Yin and Yang of opposing vectors: an explanation for side effects of biologics
Explaining arthropathy development through IL-4 and IL-13 blockade
Best of the Posters
Potential biomarker discovered for treatment response to ustekinumab
TNF inhibitor for immune-mediated inflammatory disease doubles the risk of paradoxical psoriasis
Secukinumab also tolerable in paediatric psoriasis patients
High treatment success with ixekizumab in patients with psoriasis and diabetes
Related Articles

November 29, 2021
ICD 2021 Highlights Podcast
December 17, 2020
Biologic psoriasis treatment and COVID-19 risk: Contradictory results
August 6, 2020
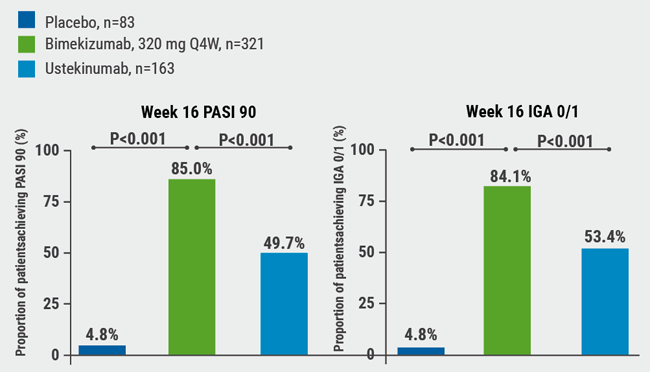
IL-17A and IL-17F blockade remarkably effective in psoriasis
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

