The Psoriasis Patient Registry for Outcomes, Therapy and Epidemiology of COVID-19 Infection (PsoProtect) was created early on during the pandemic in March 2020 to learn about the effect of SARS-Cov-2 infection on patients with psoriasis [1,2]. PsoProtect collects data from clinicians, who provide detailed data on their psoriasis patients with confirmed or suspected COVID-19 on a global online platform. Prof. Catherine Smith (King’s College London, UK) reported the latest findings from a data-cut in July 2021 that included 1,272 cases [1].
The cohort consisted of 40% women, had a mean age of 49 years, and 86% were White. Systemic treatment was given to 87% of the patients, with 70% receiving biologics. “We found that, as in our earlier analysis, risk factors associated with hospitalisation in people with psoriasis are the same as in the general population: male sex, age, non-White ethnicity, and comorbidities,” Prof. Smith stated. Concerning comorbidities, significantly increased likelihoods of hospitalisation were seen for hypertension (odds ratio [OR] 1.81; 95% CI 1.18–2.78), chronic liver disease (OR 2.48; 95% CI 1.37–4.48), and chronic lung disease (OR 2.5; 95% CI 1.41–4.43). Also, patients on non-biologic immunosuppression, mostly with methotrexate, acitretin, or apremilast, were more prone to hospitalisation than those on biologics (OR 2.37; 95% CI 1.5–3.76).
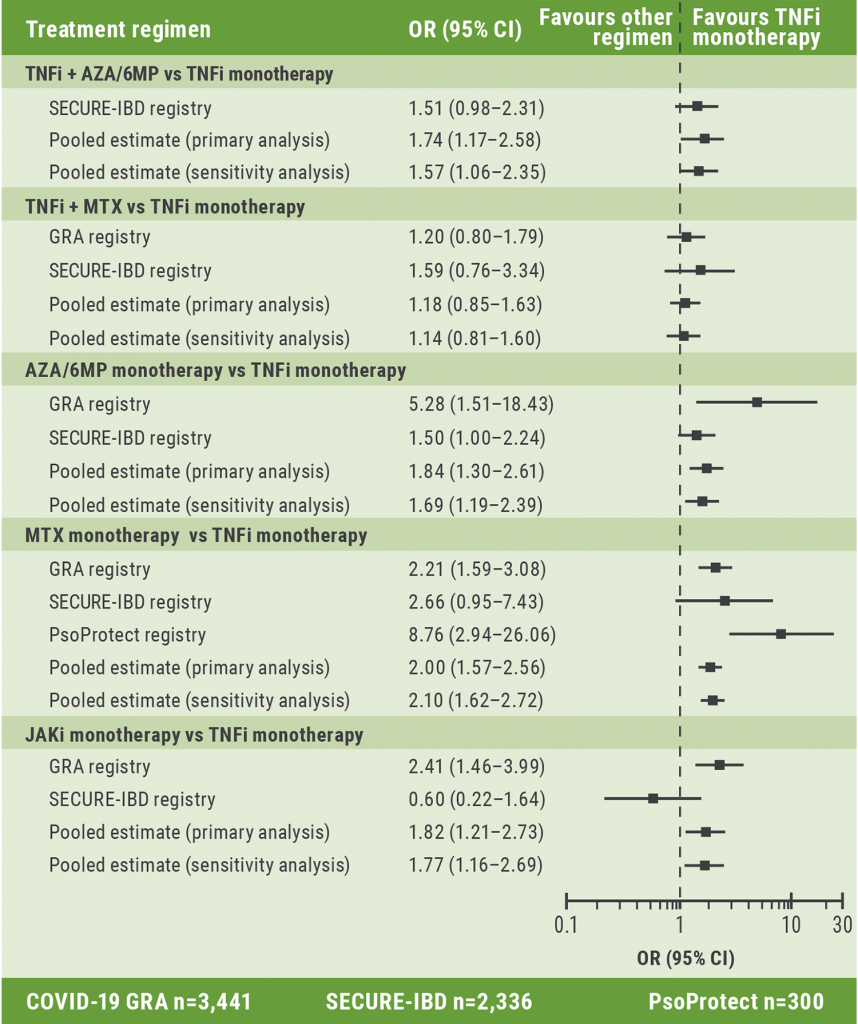
To achieve the necessary amount of statistical power to differentiate between treatment regimens, PsoProtect sought collaboration with registries of other immune‐mediated inflammatory diseases. This led to pooled data of over 6,000 patients with psoriasis, rheumatologic diagnoses, and inflammatory bowel disease. The analysis that assessed the risk of hospitalisation for COVID-19 or death suggested that anti-TNF monotherapy was protective compared with standard systemic immunotherapy. Prof. Smith stressed that it was reassuring that findings seemed to be consistent across all 3 registries. The pooled analysis of risk for hospitalisation or death in patients with suspected and confirmed COVID-19 led to an OR of 2.0 (95% CI 1.57–2.56) for methotrexate monotherapy versus TNF-inhibitor monotherapy (see Figure). The sensitivity analysis, comprising only confirmed cases, resulted in an OR of 2.1 (95% CI 1.62–2.72) for the same comparison (see Figure). “But these findings need to be interpreted with caution: first, this is an association and not causation, but also the reporting of patients through these registries is subject to bias and findings really do need to be validated in population-based data sets,” Prof. Smith pointed out.
Figure: Comparison of the likelihood for COVID-19 hospitalisation or death in psoriasis patients treated with immunomodulatory therapy versus TNF monotherapy (adjusted odds ratios) [1,4]
The related PsoProtectMe registry consists of data from self-reports of over 4,000 patients from more than 80 countries all over the world and has different patient characteristics than PsoProtect [1,3]. The mean age of participants is 47.2 years and 62% are women. Of the 38.1% of these patients who were on systemic medication during the pandemic, 18.4% were non-adherent to their regimen. This was linked to a significantly higher risk of psoriasis worsening (OR 2.9; 95% CI 2.31–3.6). Reasons for stopping the systemic treatment included fear of COVID-19 complications.
Over 80% of PsoProtectMe participants reported receiving at least 1 dose of a COVID-19 vaccine. The 8.3% who refused to be vaccinated had overall the same reasons for this decision as the general population. Furthermore, worries about a potential worsening of their psoriasis also played an important role.
Prof. Smith concluded that “both PsoProtect and PsoProtectMe have proved extremely powerful mechanisms for very rapid accrual of data and we hope that we will be able to deploy them in the future for research.”
- Smith C. The impact of the COVID-19 pandemic on people with psoriasis: an update from the PsoProtect and PsoProtectMe global registries. FC16, Psoriasis from Gene to Clinic 2021, 9–11 December.
- PsoProtect. https://psoprotect.org/ [Last accessed 06 January 2022].
- PsoProtectMe. https://psoprotectme.org/ [Last accessed 06 January 2022].
- Izadi Z, et al. JAMA Netw Open. 2021;4(10):e2129639.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Patients on immunomodulators need 2 COVID-19 vaccinations before seroconversion Next Article
Pilot trial shows potential benefit of stem-cell therapy in microvascular dysfunction »
« Patients on immunomodulators need 2 COVID-19 vaccinations before seroconversion Next Article
Pilot trial shows potential benefit of stem-cell therapy in microvascular dysfunction »
Table of Contents: PFGC 2021
Featured articles
Letter from the Editor
Guselkumab shows highest drug survival among systemic treatments
Genes in Psoriasis and Psoriatic Arthritis
HLA-C*06:02-positive patients on ustekinumab show higher drug survival in a real-world scenario
Protective factors identified against anti-drug antibody formation to adalimumab in psoriasis
Comorbidity in Psoriasis
Psoriasis associated with a higher cancer risk
Comorbidity and clinical features of psoriasis vary according to HLA-C*06:02 status
Psoriasis patients with cardiovascular comorbidity characterised by high systemic inflammation
Psoriasis Therapy: New Findings
Inhibition of heat shock protein: A novel way to treat psoriasis?
Guselkumab shows highest drug survival among systemic treatments
Tapering biologics: No alarming signs of increased anti-drug antibodies
Intermediate monocytes are possible predictors of response to secukinumab
Gut microbiota of psoriasis patients: less diverse and reduced functionality
COVID-19: What's New
DLQI scores underestimated during lockdowns?
TNF blockers likely beneficial for psoriatic patients with COVID-19
Patients on immunomodulators need 2 COVID-19 vaccinations before seroconversion
Paradoxical Reactions to Biologics
The Yin and Yang of opposing vectors: an explanation for side effects of biologics
Explaining arthropathy development through IL-4 and IL-13 blockade
Best of the Posters
Potential biomarker discovered for treatment response to ustekinumab
TNF inhibitor for immune-mediated inflammatory disease doubles the risk of paradoxical psoriasis
Secukinumab also tolerable in paediatric psoriasis patients
High treatment success with ixekizumab in patients with psoriasis and diabetes
Related Articles
November 18, 2021
Nail psoriasis: An important target to be treated
August 26, 2022
Dose tapering in psoriasis is associated with a low relapse rate
November 18, 2021
Treating psoriasis during pregnancies
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

