The multicentre, investigator-initiated EAST-AFNET 4 trial (NCT01288352) was conducted to assess the benefits of early rhythm-control therapy compared with usual care in patients with early, recently diagnosed AF [1]. Patients with a CHA₂DS₂-VASc score of ≥2 and recent onset (≤1 year) AF were eligible for randomisation. The primary outcome was a composite of cardiovascular death, stroke, heart failure worsening, or acute coronary syndrome. The previously published results displayed clinical benefits of early rhythm control compared with usual care (HR 0.79; P=0.005) [2].
Dr Andreas Goette (St. Vincenz Hospital Paderborn, Germany) presented the prespecified analysis, which divided AF patients into 3 groups: first-diagnosed AF (n=1,048), paroxysmal AF (n=994), and persistent AF (n=743). The same composite outcome was evaluated as the first primary outcome. The second primary outcome was the number of nights spent in hospital.
After 8 years of follow-up, the clinical benefits of early rhythm control were consistent amongst all 3 subgroups (first-diagnosed AF HR 0.91; paroxysmal AF HR 0.67; persistent AF HR 0.76), without significant heterogeneity of effect between groups (P-interaction=0.39). However, the nights spent in hospital in the rhythm-control group were significantly increased in patients with first-diagnosed AF (mean 1.38/year; 95% CI 1.12–1.70) compared with patients with paroxysmal AF (0.84; 95% CI 0.67-1.03) or persistent AF (1.02; 95% CI 0.80-1.30; P-interaction=0004). Additional analysis showed that this effect was mainly driven by events that occurred within the first 10 days after diagnosis (see Figure). Notably, the risk of hospitalisation due to acute coronary syndrome was significantly increased in patients with first-diagnosed AF.
Figure: Subgroup analysis across AF subtypes and time since diagnosis [1]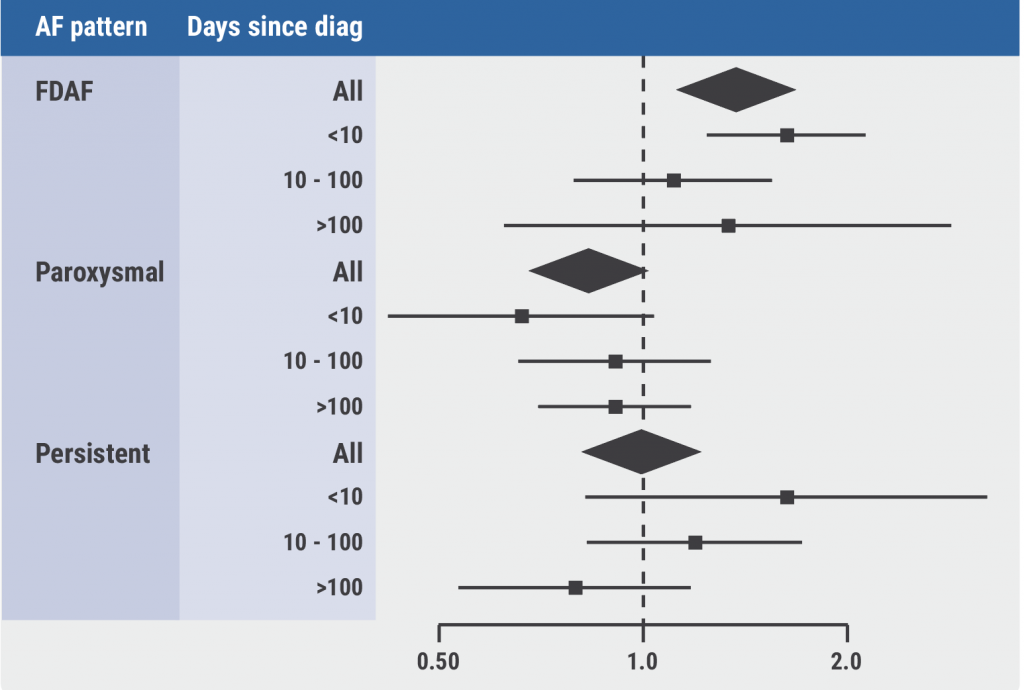 AF, atrial fibrillation; FDAF, first-diagnosed AF.
AF, atrial fibrillation; FDAF, first-diagnosed AF.
Furthermore, the 2-year EQ-5D scores for these subgroups displayed a decreased quality of life in patients with first-diagnosed AF (mean delta -2.16) compared with patients paroxysmal AF (+2.49) and persistent AF (+3.96; P=0.019). Dr Goette argued that the drop in quality of life of those with first-diagnosed AF may be related to the increased rates of hospitalisations or other events in this group. Moreover, he explained that these increased rates suggest that first-diagnosed AF may be a biomarker for concomitant cardiovascular disease; a pattern that could not be observed in patients with chronic types of AF. Careful monitoring of patients with first-diagnosed AF, especially during the first weeks after diagnosis is therefore recommended, according to Dr Goette.
- Goette A, et al. Patients with first diagnosed atrial fibrillation are at high risk for cardiovascular events and suitable for early rhythm control: The EAST-AFNET 4 trial. FS05, AHA Scientific Sessions 2021, 13–15 November.
- Kirchhof P, et al. N Engl J Med 2020;383:1305–16.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Letter from the Editor Next Article
LAA ligation did not reduce recurrent atrial arrhythmias in persistent AF »
« Letter from the Editor Next Article
LAA ligation did not reduce recurrent atrial arrhythmias in persistent AF »
Table of Contents: AHA 2021
Featured articles
The scope of remote healthcare in hypertension and hyperlipidaemia
Atrial Fibrillation
New developments in remote diagnostics and monitoring of AF
Head-to-head: Efficacy of dabigatran versus warfarin on cognitive impairment
Posterior left pericardiotomy safe and effective in reducing atrial fibrillation
LAA ligation did not reduce recurrent atrial arrhythmias in persistent AF
Equal benefits of early rhythm control in AF subtypes
CVD Risk Reduction
Remote healthcare programme improves hypertension and lipid control
Novel oral PCSK9 inhibitor shows promising results for hypercholesterolaemia
REVERSE-IT: Interim analysis shows promising effect of bentracimab on ticagrelor reversal
No significant effect of aspirin on reducing cognitive impairment
Milvexian phase 2 data supports safety and efficacy for VTE prevention after total knee replacement
Network meta-analysis observes no clear effect of eicosapentaenoic acid on CV outcomes
Heart Failure
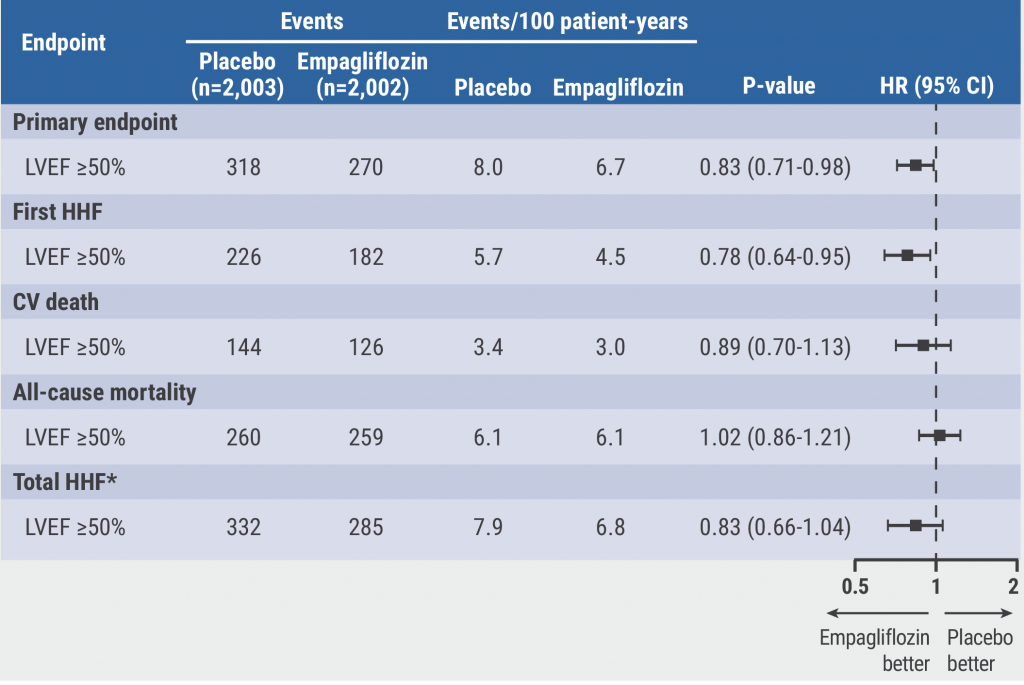
Empagliflozin efficacious in HF patients with preserved ejection fractions ≥50%
EMPULSE: Empagliflozin improves outcomes of acute heart failure
CHIEF-HF: Canagliflozin improves health status in heart failure
DREAM-HF: MPC therapy for HFrEF did not meet primary endpoint
Therapeutic approaches in heart failure with diabetes
Acute Coronary Syndrome
Ticagrelor cessation: early CABG non-inferior to delayed surgery
Distinguishing patients before AMI based on plaque morphology
Vascular Diseases: PVD
Rivaroxaban regimen beneficial after revascularisation for claudication
LIBERTY 360 shows quality-of-life improvements after peripheral vascular intervention
Deficient treatment outcomes after PVI in Black and low-income adults with PAD
REDUCE-IT: Cardiovascular risk reduction with icosapent ethyl in PAD
Vascular Diseases: CAD
Long-term reduced risk of CV events with ticagrelor plus aspirin after CABG
Early surgery outperforms conservative management in asymptomatic severe aortic stenosis
External support device for SVG grafts in CABG surgery shows promise
COVID-19 & the Heart
Blood pressure control disrupted during the pandemic
Icosapent ethyl did not reduce the risk of hospitalisation in COVID-19
Neutral effect of P2Y12 inhibitors in non-critical COVID-19 hospitalisations
COVID-19 mRNA vaccination benefits outweigh the risk for myocarditis
Other
2021 Guideline for Chest Pain: Top 10 takeaways
Accurate ejection fraction assessment in paediatric patients via artificial intelligence
Concomitant tricuspid annuloplasty reduces treatment failure in moderate tricuspid regurgitation
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com