Top 10 takeaways
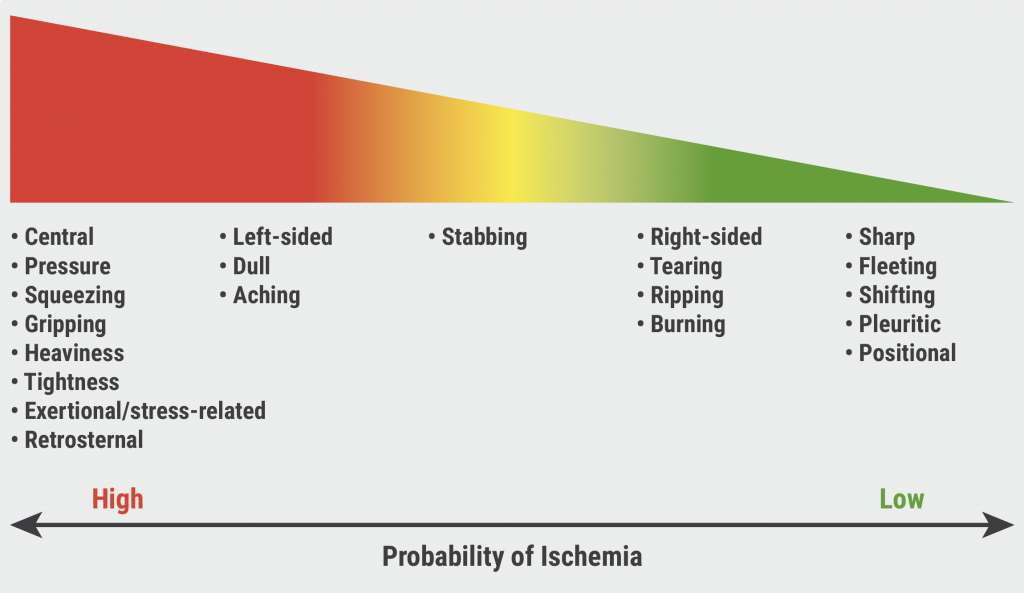
- Chest pain is more than pain in the chest. The shoulder area, jaw, epigastric area, neck, or back are included in the chest pain spectrum. Physicians should perform an initial assessment of chest pain to estimate the likelihood of symptoms being related to myocardial ischaemia (class 1) (see Figure).
- High-sensitivity cardiac troponin (hs-cTn) enables swift detection or exclusion of myocardial injury. Thus, hs-cTn is the preferred biomarker in patients presenting with acute chest pain (class 1). In addition, physicians need to be acquainted with the analytical performance and the 99th percentile upper reference limit that defines myocardial injury for the cTn assay at their facility (class 1).
- Patients presenting with symptoms of life-threatening causes of acute chest pain need to be transported to the ED with urgency, ideally by emergency medical services (class 1). Patients with stable chest pain should receive an ECG, unless a non-cardiac cause is apparent (class 1).
- In patients with acute chest pain and possible acute coronary syndrome (ACS) who have a low-risk profile, shared decision-making facilitates risk communication and increases understanding (class 1). Moreover, shared decision-making does not hamper outcomes.
- Patients who present with acute or stable chest pain and have a low-risk profile do not need to be tested routinely (class 1). Prof. Gulati emphasised this recommendation as the most important one in the new guideline.
- Patients with acute chest pain and possible ACS should be categorised in low-, intermediate-, and high-risk profiles by means of clinical decision pathways (CDPs) (class 1). Available clinical test results should be incorporated into the CDPs (class 1).
- Women with chest pain are at risk for underdiagnosis. Thus, it is recommended to assess for accompanying symptoms that are more prevalent in women with ACS, such as shortness of breath and nausea (class 1).
- Patients who are most likely to benefit from (further) testing should be identified. The chest guideline included CDPs to aid clinicians in the decision-making.
- The description of chest pain as ‘atypical’ is not helpful. Instead, chest pain should be classified as cardiac, possibly cardiac, or non-cardiac, since these terms are more specific to the underlying diagnosis (class 1).
- Finally, evidence-based diagnostic protocols should be used for the assessment of coronary artery disease and adverse events in patients with acute or stable chest pain, establishing a structured risk assessment.
- Gulati M, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain. CS.ME.495, AHA 2021 Scientific Sessions, 13–15 November.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Accurate ejection fraction assessment in paediatric patients via artificial intelligence Next Article
Transcatheter pulmonary-valve replacement, surgery appear to have comparable outcomes »
« Accurate ejection fraction assessment in paediatric patients via artificial intelligence Next Article
Transcatheter pulmonary-valve replacement, surgery appear to have comparable outcomes »
Table of Contents: AHA 2021
Featured articles
The scope of remote healthcare in hypertension and hyperlipidaemia
Atrial Fibrillation
New developments in remote diagnostics and monitoring of AF
Head-to-head: Efficacy of dabigatran versus warfarin on cognitive impairment
Posterior left pericardiotomy safe and effective in reducing atrial fibrillation
LAA ligation did not reduce recurrent atrial arrhythmias in persistent AF
Equal benefits of early rhythm control in AF subtypes
CVD Risk Reduction
Remote healthcare programme improves hypertension and lipid control
Novel oral PCSK9 inhibitor shows promising results for hypercholesterolaemia
REVERSE-IT: Interim analysis shows promising effect of bentracimab on ticagrelor reversal
No significant effect of aspirin on reducing cognitive impairment
Milvexian phase 2 data supports safety and efficacy for VTE prevention after total knee replacement
Network meta-analysis observes no clear effect of eicosapentaenoic acid on CV outcomes
Heart Failure
Empagliflozin efficacious in HF patients with preserved ejection fractions ≥50%
EMPULSE: Empagliflozin improves outcomes of acute heart failure
CHIEF-HF: Canagliflozin improves health status in heart failure
DREAM-HF: MPC therapy for HFrEF did not meet primary endpoint
Therapeutic approaches in heart failure with diabetes
Acute Coronary Syndrome
Ticagrelor cessation: early CABG non-inferior to delayed surgery
Distinguishing patients before AMI based on plaque morphology
Vascular Diseases: PVD
Rivaroxaban regimen beneficial after revascularisation for claudication
LIBERTY 360 shows quality-of-life improvements after peripheral vascular intervention
Deficient treatment outcomes after PVI in Black and low-income adults with PAD
REDUCE-IT: Cardiovascular risk reduction with icosapent ethyl in PAD
Vascular Diseases: CAD
Long-term reduced risk of CV events with ticagrelor plus aspirin after CABG
Early surgery outperforms conservative management in asymptomatic severe aortic stenosis
External support device for SVG grafts in CABG surgery shows promise
COVID-19 & the Heart
Blood pressure control disrupted during the pandemic
Icosapent ethyl did not reduce the risk of hospitalisation in COVID-19
Neutral effect of P2Y12 inhibitors in non-critical COVID-19 hospitalisations
COVID-19 mRNA vaccination benefits outweigh the risk for myocarditis
Other
2021 Guideline for Chest Pain: Top 10 takeaways
Accurate ejection fraction assessment in paediatric patients via artificial intelligence
Concomitant tricuspid annuloplasty reduces treatment failure in moderate tricuspid regurgitation
Related Articles

November 30, 2021
AHA 2021 Highlights Podcast

© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

