The PHERGAIN trial, presented by Javier Cortés, MD, PhD, of the Vall d´Hebron Institute of Oncology, in Barcelona, included 356 patients with stage I-IIIA HER2-positive breast cancer. They were randomly assigned 1:4 to receive docetaxel and carboplatin along with trastuzumab and pertuzumab (TCHP; Arm A, 71 patients), or trastuzumab and pertuzumab without chemotherapy but with endocrine therapy in the presence of an estrogen receptor–positive tumor (Arm B, 285 patients). The Figure outlines the study schema.
Patients underwent a PET scan after two cycles of therapy; in Arm B, responders (defined as a SUVmax reduction of at least 40%) received six cycles of dual HER2 blockade (trastuzumab/pertuzumab with endocrine therapy), while nonresponders received six cycles of the TCHP regimen. Following surgery, PET responders in Arm B who achieved a pCR received dual HER2 blockade for up to 1 year, meaning they never received chemotherapy; those without a pCR received TCHP followed by dual HER2 blockade.
A total of 79.6% of those evaluated by PET imaging were responders. Of those, 37.9% achieved a pCR, which Dr. Cortés said meant that the null hypothesis can be rejected (p < 0.001). The pCR rate among patients in Arm B who were nonresponders was 25.9%.
In all 285 patients in Arm B, the pCR rate was 35.4%; in Arm A, where all patients received chemotherapy, it was 57.7% (p < 0.01). In Arm A, 65.6% of those who were responders on the PET scan achieved a pCR, compared with 10% of those who were nonresponders (p < 0.01).
There were no significant differences with regard to breast-conserving surgery between the two arms, or between PET responders and nonresponders.
In Arm A, 58.8% of patients had a grade 3/4 treatment-related adverse event (AE); in Arm B nonresponders, who also received chemotherapy, that rate was 44.6%. In contrast, only 1.3% of PET responders in Arm B had such an AE. No patients who did not receive chemotherapy discontinued treatment due to an AE.
Depending on results from an ongoing evaluation of 3-year invasive disease-free survival (iDFS), Dr. Cortés said, “this strategy could select a group of HER2-positive early breast cancer patients who would not need chemotherapy.”
Sara A. Hurvitz, MD, of the David Geffen School of Medicine at the University of California, Los Angeles, was the discussant for the abstract. She highlighted the “outstanding” adverse event rate in those who did not receive chemotherapy. “I think PET imaging after several cycles of therapy is very promising to assess the tumor responsiveness,” she said, adding that it will be important to see the iDFS rate.
Figure. PHERGAIN Study Design [1]
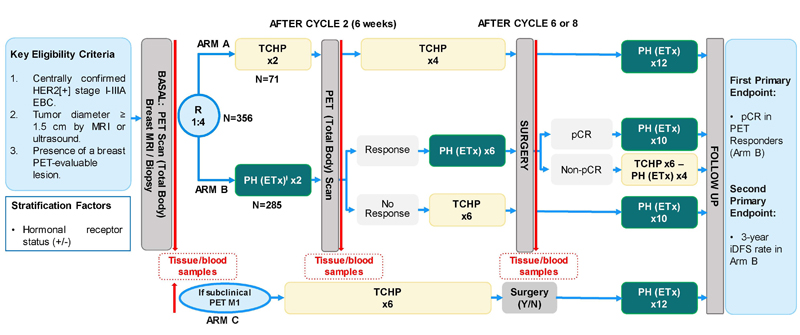
Abbreviations: C, carboplatin; D, docetaxel; EBC, early breast cancer; ETx, endocrine therapy (letrozole post-menopausal/tamoxifen pre-menopausal) adjuvant ETx up to 3 years from surgery; PET, 18F-fluorodeoxyglucose positron emission tomography/computed tomography; H, trastuzumab SC; HER2, human epidermal growth factor receptor 2; iDFS, invasive disease-free survival; MRI, magnetic resonance imaging; P, pertuzumab IV; R, randomization; TCHP, trastuzumab, pertuzumab, docetaxel, and carboplatin.ⱡAll hormonal receptor-positive patients will receive ETx concomitantly with PH (except on chemotherapy).*PET Responders: RECIST responders after cycle 2 with SUVmax reduction ≥40%*Pathological complete response (ypT0/isN0)- Cortes J, et al. ASCO Virtual Meeting, 29-31 May 2020, Abstract
Posted on
Previous Article
« Letter from the Editor Next Article
BYLieve demonstrates efficacy of PIK3CA-directed treatment post CDK4/6-ihibition »
« Letter from the Editor Next Article
BYLieve demonstrates efficacy of PIK3CA-directed treatment post CDK4/6-ihibition »
Table of Contents: ASCO 2020
Featured articles
COVID-19 & Telemedicine
COVID-19 and Cancer Consortium Registry: initial results
Oncology hospital-at-home model reduces hospitalizations, emergency department visits, and costs
Nurse-led telephone triage system reduces hospitalizations, helps patients manage symptoms at home
Melanoma
Adjuvant pembrolizumab: durable RFS for stage III melanoma
Adjuvant pembrolizumab: durable RFS for stage III melanoma
Pembrolizumab plus low-dose ipilimumab well tolerated after progression on PD1 antibody therapy
Toripalimab plus axitinib effective in metastatic mucosal melanoma
Breast & Ovarian Cancer
Advanced breast cancer: locoregional therapy does not improve OS
T-DM1 does not improve safety or efficacy in HER-2 positive early breast cancer; favorable iDFS reported
Maintenance olaparib improves OS in relapsed ovarian cancer with BRCA1/2 mutation
Combination pembrolizumab/chemo improves PFS in metastatic TNBC
Effect of veliparib with or without cisplatin in breast cancer: results of SWOG S1416
PHOEBE, a phase 3 trial comparing pyrotinib and lapatinib in HER2-positive metastatic breast cancer
BYLieve demonstrates efficacy of PIK3CA-directed treatment post CDK4/6-ihibition
Strategies emerge for chemotherapy de-escalation in HER2-positive breast cancer
Multiple Myeloma
Carfilzomib: no PFS benefit for multiple myeloma
Lung Cancer
ES-SCLC: tremelimumab + durvalumab + chemotherapy misses endpoint
Adjuvant osimertinib in NSCLC: practice changing ADAURA trial
ES-SCLC: pembrolizumab KEYNOTE-604 data
Second-line gemcitabine plus ramucirumab significantly improves overall survival
Tiragolumab and atezolizumab: ORR in NSCLC
MET-amplified advanced NSCLC responds well to MET inhibitor capmatinib
Genitourinary Cancer
Urothelial cancer: avelumab works as maintenance therapy
ARAMIS final OS and nmCRPC safety outcomes
Final survival results from phase 3 SPARTAN trial
Novel drug for kidney cancers/VHL patients
Primary analysis from IMvigor010, adjuvant atezolizumab in high risk muscle-invasive urothelial carcinoma
First randomised trial of Lu-PSMA in mCRPC progressing after docetaxel
Gastrointestinal Cancer
HER2-expressing metastatic colorectal cancer: trastuzumab deruxtecan
REGOMUNE: a phase 2 study combining regorafenib and avelumab
Cardiotoxicity: consider switching to S-1
Perioperative chemotherapy for resectable pancreatic ductal adenocarcinoma
Real-world data of sequential sorafenib followed by regorafenib in unresectable HCC
Paediatric Cancer
Sustained improvements in quality of life with larotrectinib
Promising first immunotherapy trial in placental trophoblastic tumours
Precision medicine for poor-prognosis paediatric patients
Related Articles

September 17, 2020
Urothelial cancer: avelumab works as maintenance therapy

September 9, 2020
Promising first immunotherapy trial in placental trophoblastic tumours
September 8, 2020
ES-SCLC: pembrolizumab KEYNOTE-604 data
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

