Although the use of NOACs has risen considerably over the last years, VKAs are still the most frequently prescribed oral anticoagulants worldwide. They work by inhibiting vitamin K1, which is necessary to produce coagulation factors. However, VKA also inhibit vitamin K2, which plays an essential role in activating the matrix Gla protein, which acts as a strong local inhibitor of arterial calcifications. Dr Selma Hasific (Odense University, Denmark) and colleagues aimed to investigate whether treatment with VKA is associated with coronary artery calcification in individuals who had no prior cardiovascular disease. This was done by collecting data on cardiovascular risk factors and coronary artery calcifications scores from cardiac CT scans performed as part of clinical examinations (n=9,672) or research studies (n=14,166) in the period 2007-2017. Included in the study were 17,254 participants (median 67 years old, 75% males) with no prior cardiovascular disease (10% had been treated with VKA and 7% with NOAC).
For patients who were treated for a longer period with VKA, treatment was associated with higher coronary artery calcifications categories. For each cumulative year of VKA treatment, the odds increased of being in a higher coronary artery calcifications category (i.e. having more severe atherosclerosis). The odds ratio was 1.032. All traditional cardiovascular risk factors were also associated with coronary artery calcifications. Contrarily, NOAC treatment duration was not associated with coronary artery calcification category (OR=1.002). In a sensitivity analysis of patients without statin treatment (n=12,143), the association between VKA treatment and coronary artery calcification category remained unchanged. Finally, no significant interaction was observed between VKA treatment duration and age on coronary artery calcification category [1].
1. Hasific S, et al. Risk of arterial calcification by conventional vitamin K antagonist treatment. Abstract 456. ESC Congress 2019, 31 Aug-4 Sept, Paris, France.
Posted on
Previous Article
« Long-term data confirm superiority of inter-hospital transport for primary PCI vs fibrinolysis Next Article
Early vasodilation in acute HF does not improve outcomes »
« Long-term data confirm superiority of inter-hospital transport for primary PCI vs fibrinolysis Next Article
Early vasodilation in acute HF does not improve outcomes »
Related Articles
February 18, 2021
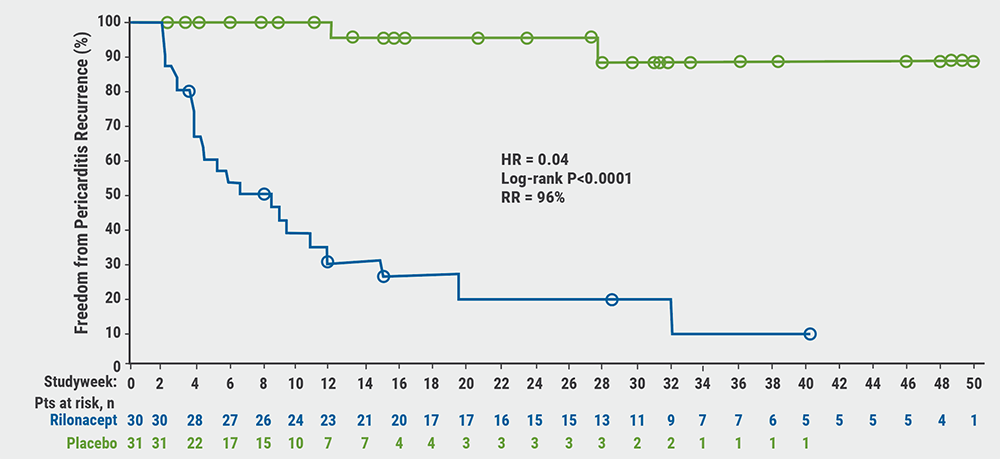
Rilonacept reduces risk of pericarditis recurrence
November 9, 2021
Psychological stress exacts high toll on adults with heart disease
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

