Infants born prematurely have impaired capacity to deal with oxidative stress shortly after birth. Particulate matter with a diameter >10 μm (PM10) and NO2 are known oxidative stressors to airways and lungs. Therefore, Ms Fabienne Decrue (University of Basel, Switzerland) and colleagues investigated whether preterm infants are more susceptible to pre- and postnatal exposure to air pollution in comparison to term infants, and if this is reflected in altered postnatal lung function [1,2].
Infants from the Basel-Bern infant lung development (BILD) cohort born between 1999–2017 were included. Individual air pollution (expressed in PM10 and NO2) exposure was calculated individually for each infant during the second trimester of pregnancy and postnatal. The primary outcome was postnatal lung function at 33 weeks postconceptional age, expressed as tidal breathing flow volume loops and exhaled surrogate markers of inflammation, and oxidative stress response (fractional exhaled nitrogen oxide, FeNO).
Within this study, 771 infants were included over a period of 18 years, of which one third were preterm infants (n=254). Preterm infants were divided over 2 groups: moderate-to-late preterm infants (32–37 weeks) and extreme preterm infants (<31 weeks). Significant associations of increases in PM10 during pregnancy were found for minute ventilation, tidal volume, and FeNO (see Figure). Associations of air pollution and FeNO differed significantly between preterm and term infants (P=0.006).
Figure: Lung function as a result of PM10 [1]
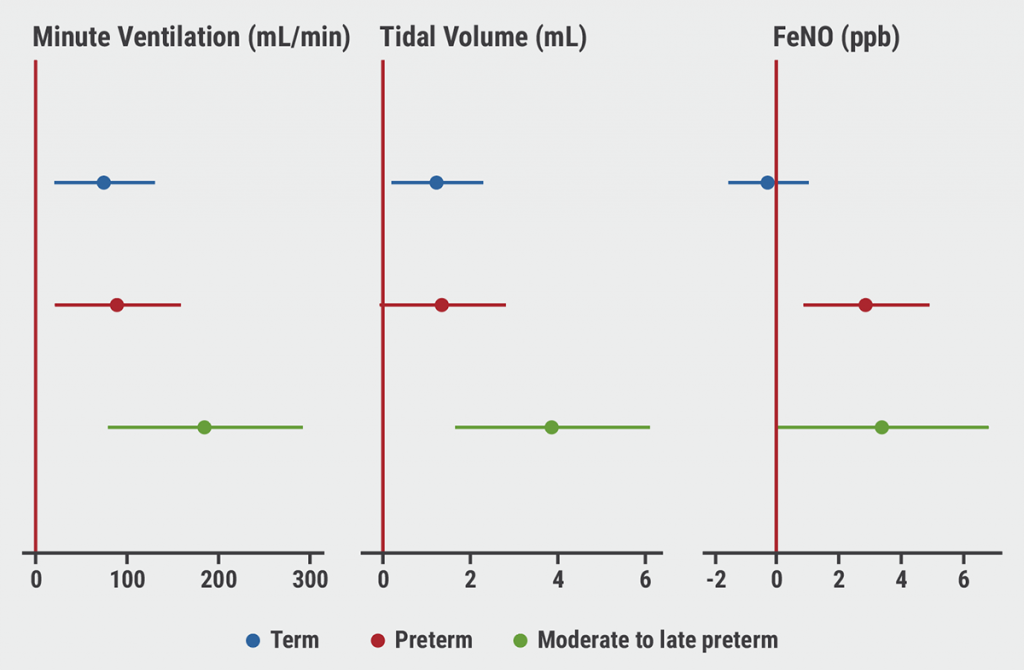
Ms Decrue was able to show that prenatal exposure to air pollution, especially during the second trimester of pregnancy, was associated with impaired infant lung function. Moreover, it was demonstrated for the first time that enhanced effects in preterm infants are suggestive of an amplified susceptibility indicating that air pollution measures should be taken to prevent populations at risk, even in low-to-moderate polluted areas such as Switzerland.
- Decrue F, et al. Increased impact of air pollution on lung function in preterm vs. term infants: the BILD study. Abstract 2958. ERS 2021, 5–8 September.
- Decrue F, et al. Am J Respir Crit Care Med. 2021 Sep 29.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Biomarkers do not discriminate severe from severe uncontrolled asthma Next Article
No immunological parameters identified for Down syndrome children »
« Biomarkers do not discriminate severe from severe uncontrolled asthma Next Article
No immunological parameters identified for Down syndrome children »
Table of Contents: ERS 2021
Featured articles
Letter from the Editor
COVID-19 Research: Looking Back and Moving Forward
Higher inflammation markers in COVID-19 patients with a first negative PCR test
Persistent fatigue following COVID-19
Risk of COVID-19-related morbidity and mortality in young and middle-aged adults
Respiratory Viral Infections: Insights from Recent Studies
Rhinovirus bronchiolitis increased risk of recurrent wheezing and asthma
COPD: Evidence Update
Livestock farming affected the airway microbiome of COPD patients
Reduction of COPD severe acute exacerbations by candidate vaccine
Paediatrics and Vaccinology
Better lung function in children with a healthy diet
Need for validated severity score in the assessment of bronchiolitis
Increased impact of air pollution on lung function in preterm infants
Pearls in Asthma Research
Biomarkers do not discriminate severe from severe uncontrolled asthma
Increased blood neutrophiles in patients with obesity and asthma
Blood inflammatory phenotypes associated with clinical symptoms of asthma
Related Articles
August 17, 2022
Switching biologicals in severe asthma
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

