Asthma is a heterogenous disease characterised by various phenotypes, including inflammatory ones. In blood and sputum samples, 4 different phenotypes have been identified based on the results of the Environment of Asthma (EGEA) case control study: eosinophilic, neutrophilic, paucigranulocytic, and mixed phenotypes. Cut-offs of 250 and 500 cells/mm3 have been suggested for eosinophils and neutrophils, respectively. However, these asthma inflammatory phenotypes have not been verified in population-based studies. Therefore, the current study, presented by Dr Tajidine Tsiavia (University of Paris-Saclay, France) aimed to identify and characterise the 4 phenotypes in adults from the largest French population-based ‘Constances’ cohort [1].
From 2012 to 2019, participants aged 18 to 69 years were randomly selected from the database of the National Pension Insurance Fund and invited to participate in the study. Data from questionnaires and white blood cell (WBC) counts at moment of inclusion was analysed. Current asthma was defined by the report of asthma attacks, respiratory symptoms, or use of asthma medication in the past 12 months. Inflammatory phenotypes were defined based on the EGEA cut-offs, as mentioned before. Statistical analyses included logistic regression models adjusted for age, sex, BMI, smoking, education level, French deprivation index, and asthma treatment.
Clinical data was available from 192,648 patients, from which 160,272 patients were selected that matched the inclusion criteria. Of these participants, 15,019 (9.4%) reported current asthma. Phenotypes differed significantly by age, sex, BMI, smoking, education level, and asthma treatment.
The neutrophilic, eosinophilic, and mixed phenotypes were positively associated with several clinical variables (see Figure). The neutrophilic phenotype was associated with being woken by an attack of coughing, chronic bronchitis, and dyspnoea (aOR ranging from 1.21 to 1.42). The eosinophilic and mixed phenotypes were associated with asthma attacks (aOR 1.31; 95% CI 1.20–1.42 and aOR 1.25; 95% CI 1.02–1.53, respectively) and asthma symptom score (P<0.001). The eosinophilic phenotype was also associated with being woken with chest tightness (aOR 1.30 95% CI 1.20–1.40). The distribution of asthma phenotypes differed by age (P<0.0001). Data for the paucigranulocytics was not shown.
Figure: Associations between inflammatory phenotypes and clinical characteristics of asthma [1]
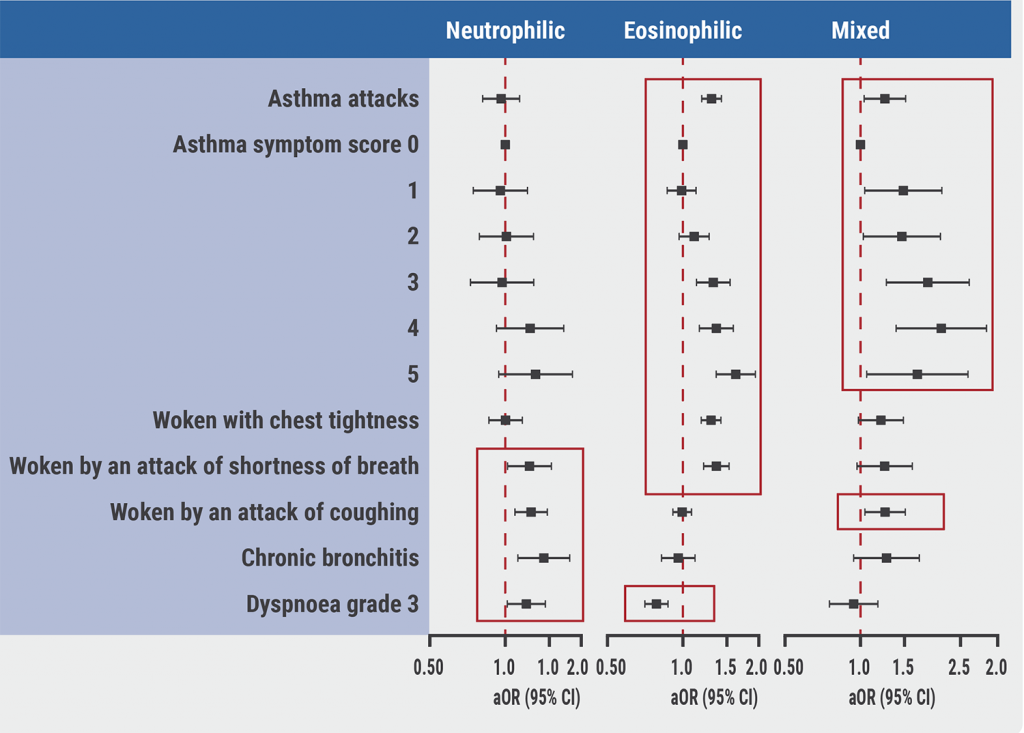
Positive associations are outlined in red.
In conclusion, clinical differences were found between blood inflammatory phenotypes in a large population-based cohort. Similar differences have been described in clinical and case-control studies. Blood inflammatory phenotypes may be helpful in better understanding the pathophysiology of asthma and in guiding treatment.
- Tsiavia T, et al. Blood inflammatory phenotypes in asthma in the Constances cohort. Abstract 4217. ERS 2021, 5–8 September.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« New class of CAR-T promising against neuroblastoma, other solid tumors Next Article
Magnesium supplements improved lung function in asthma patients »
« New class of CAR-T promising against neuroblastoma, other solid tumors Next Article
Magnesium supplements improved lung function in asthma patients »
Table of Contents: ERS 2021
Featured articles
Letter from the Editor
COVID-19 Research: Looking Back and Moving Forward
Higher inflammation markers in COVID-19 patients with a first negative PCR test
Persistent fatigue following COVID-19
Risk of COVID-19-related morbidity and mortality in young and middle-aged adults
Respiratory Viral Infections: Insights from Recent Studies
Rhinovirus bronchiolitis increased risk of recurrent wheezing and asthma
COPD: Evidence Update
Livestock farming affected the airway microbiome of COPD patients
Reduction of COPD severe acute exacerbations by candidate vaccine
Paediatrics and Vaccinology
Better lung function in children with a healthy diet
Need for validated severity score in the assessment of bronchiolitis
Increased impact of air pollution on lung function in preterm infants
Pearls in Asthma Research
Biomarkers do not discriminate severe from severe uncontrolled asthma
Increased blood neutrophiles in patients with obesity and asthma
Blood inflammatory phenotypes associated with clinical symptoms of asthma
Related Articles
July 18, 2022
Novel PDE4B inhibitor offers breakthrough for IPF
November 28, 2019
Female COPD patients frequently suffer from anxiety and depression
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

