The diagnostic delay of CTEPH after acute PE is over 1 year and associated with increased mortality. Dr Gudula Boon (Leiden University Medical Center, the Netherlands) and her colleagues developed a non-invasive screening strategy comprising a 'CTEPH prediction score' and 'CTEPH rule-out criteria' aimed at diagnosing CTEPH earlier and limiting the number of required echocardiograms. “Six predictors [e.g. unprovoked PE, hypothyroidism, and diagnostic delay >2 weeks] have been identified that are highly probable for CTEPH and we included them in our score,” Dr Boon explained. The CTEPH rule-out criteria were only applied on low-risk patients with a presence of CTEPH-specific symptoms. According to these criteria, patients with at least 1 ECG criteria and/or abnormal NT-proBNP values were referred to echocardiography. Included were 424 patients from 6 hospitals in the Netherlands, Poland, and Belgium. Of these participants, 69% were judged low-risk and 31% high-risk. Of all participants, 48% were low-risk patients without CTEPH-specific symptoms, and 21% were low-risk patients with symptoms.
Successful identification of almost all CTEPH patients
The algorithm successfully ruled out 342 of 343 patients (see Figure). One missed case by the algorithm translates into a failure rate of 0.29%. “There was only 1 missed case who had persistent symptoms. However, this patient would also have been missed if echocardiography had been performed initially,” Dr Boon explained. With the algorithm, CTEPH was diagnosed within 4 months after the index PE diagnosis, which is less diagnostic delay than the average. In addition, echocardiography was avoided in 81% of patients.
Figure: CTEPH screening algorithm applied at 3 months after diagnosis and 2-year follow-up results [1]
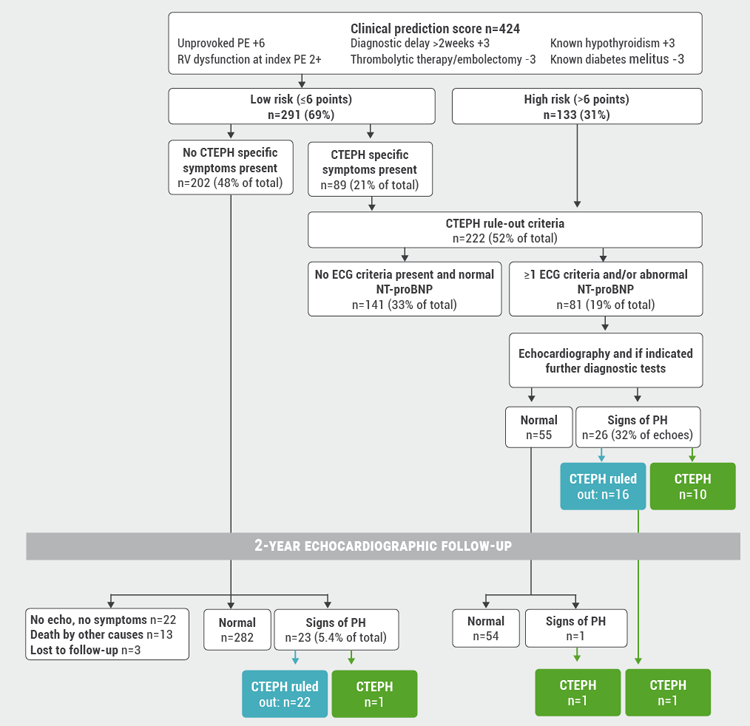
CTEPH, chronic thromboembolic pulmonary hypertension; ECG, electrocardiography; NT-proBNP, N-terminal pro-brain natriuretic peptide; PE, pulmonary embolism; PH, pulmonary hypertension; RHC, right heart catheterisation; RV, right ventricular.
1 Boon G, et al. OC.10.3, ISTH Virtual Congress 2020, 12-14 July.
Posted on
Previous Article
« Risk of checkpoint inhibitor-associated thromboembolic events important for cancer prognosis Next Article
Residual pulmonary obstruction may predict risk of VTE recurrence »
« Risk of checkpoint inhibitor-associated thromboembolic events important for cancer prognosis Next Article
Residual pulmonary obstruction may predict risk of VTE recurrence »
Table of Contents: ISTH 2020
Featured articles
Haemophilia and Rare Bleeding Disorders
Novel gene therapy leads to normal FIX activity levels in severe haemophilia B
Haemophilia gene therapy: progress and obstacles
Recombinant factor VIII safe and effective in PUPs A-LONG study
What’s New in Anticoagulation
Finding the sweet spot of anticoagulation in AF patients with ACS
Lower embryopathy risk with DOAC versus VKA during pregnancy
Higher thrombotic risk in NSCLC patient with ALK rearrangement
COVID-19 and Thrombosis
Crosstalk between inflammation and coagulation in severe COVID-19 infections
COVID-19 associated with higher VTE rates relative to influenza
Therapeutic anticoagulation not associated with lower mortality rates in COVID-19 ICU patients
COVID-19 not associated with heightened VTE risk after discharge
What’s New in Venous Thromboembolism
Residual pulmonary obstruction may predict risk of VTE recurrence
Less diagnostic delay in CTEPH diagnosis with novel algorithm
Risk of checkpoint inhibitor-associated thromboembolic events important for cancer prognosis
Pearls of the Posters
Surgical bleeding risk most important determinant of bleeding outcomes
Similar bleeding rates in patients with VTE and AF treated with DOACs
Physical rehabilitation improves health outcomes after pulmonary embolism
Guidelines adherence reduces bleeding risk after surgery and childbirth for VWD patients
Factor V Leiden mutation linked to atrial fibrillation
Increased rates of arterial thromboembolism in cancer patients
Related Articles
September 8, 2020
Finding the sweet spot of anticoagulation in AF patients with ACS
September 8, 2020
Factor V Leiden mutation linked to atrial fibrillation
September 8, 2020
Similar bleeding rates in patients with VTE and AF treated with DOACs
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

