For this study, data was collected from the registry of biological therapies of the University of Verona. Daily air pollution data (2013–2018) of the Verona area and data on RMD patients within this area were examined. The case-crossover analysis included the patients who had experienced a stable period of ≥6 months of bDMARD therapy with ≥1 low disease activity (LDA) visit plus a treatment switch or swap visit (flare visit) due to drug inefficacy (n=280). Patients who switched or swapped bDMARDs due to adverse events or drug intolerance were excluded from further analysis. Air pollution concentrations of the 60-day periods prior to the LDA visit and the flare visit were compared.
The results demonstrated that the mean concentrations of air pollutants were significantly higher prior to the flare visit compared with the LDA visit (P<0.001). In addition, ROC curves demonstrated that the combination of LDA and air pollution was a better predictor for therapy switch or swap than LDA alone. Dr Giovanni Adami (University of Verona, Italy) emphasised that these results show a direct association between environmental air pollution and a poor response to bDMARDs in RMD patients. “The ROC curves show that air pollution is an independent predictor of response to bDMARDs. When considering 100 bDMARD therapy switches or swaps, approximately 5 of them can be ascribed to the sole effect of air pollution.” This interesting work certainly needs replication in larger cohorts.
- Adami G, et al. Air pollution is a predictor of poor response to biological therapies in chronic inflammatory arthritides. POS0644, EULAR 2021 Virtual Congress, 2–5 June.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« PET/CT is a reliable measure of disease activity in LVV, but does not predict future relapses Next Article
SELECT-AXIS: 64-week results of upadacitinib in active ankylosing spondylitis »
« PET/CT is a reliable measure of disease activity in LVV, but does not predict future relapses Next Article
SELECT-AXIS: 64-week results of upadacitinib in active ankylosing spondylitis »
Table of Contents: EULAR 2021
Featured articles
COVID-19 Update
Rituximab or JAK inhibitors increase the risk of severe COVID-19
Updates on COVID-19 vaccines in patients with rheumatic disease
Immunomodulatory therapies for severe COVID-19: literature update
New Developments in Rheumatoid Arthritis
JAK inhibitors and bDMARDs not associated with increased risk of serious infections in RA
Remote management of RA is a feasible alternative for outpatient follow-up
TOVERA: Ultrasound is a promising biomarker of early treatment response
The risks of polypharmacy in RA
ABBV-3373: A potential new therapeutic agent for RA
JAK inhibitors and bDMARDs show comparable effectiveness
Spondyloarthritis: Progression in Therapies
SELECT-AXIS: 64-week results of upadacitinib in active ankylosing spondylitis
Guselkumab efficacious in PsA patients with inadequate response to TNF inhibition
Faecal microbiota transplantation not effective in active peripheral PsA
Risankizumab meets primary and ranked secondary endpoints in PsA
Prognostic factors for minimal disease activity in early psoriatic arthritis revealed
Imaging in Large-Vessel Vasculitis
PET/CT is a reliable measure of disease activity in LVV, but does not predict future relapses
Ultrasound is useful for disease monitoring in giant cell arteritis
Prevention in Rheumatic Diseases
Air pollution predicts decreased response to biological treatment in rheumatic diseases
Passive smoking associated with an increased risk of RA
Gene-Environment Interaction in Gout
Gene-diet and gene-weight interactions associated with the risk of gout
What Is New in Systemic Lupus Erythematosus
Intensified treatment regimen of anifrolumab for lupus nephritis is promising
Systemic lupus erythematosus: increased risk of severe infection
Juvenile Idiopathic Arthritis and Osteoarthritis
Efficacy and safety of secukinumab in juvenile idiopathic arthritis
Emerging therapies and future treatment directions in osteoarthritis
Related Articles
February 4, 2020
Opioids: no quality of life benefits for OA patients
February 4, 2020
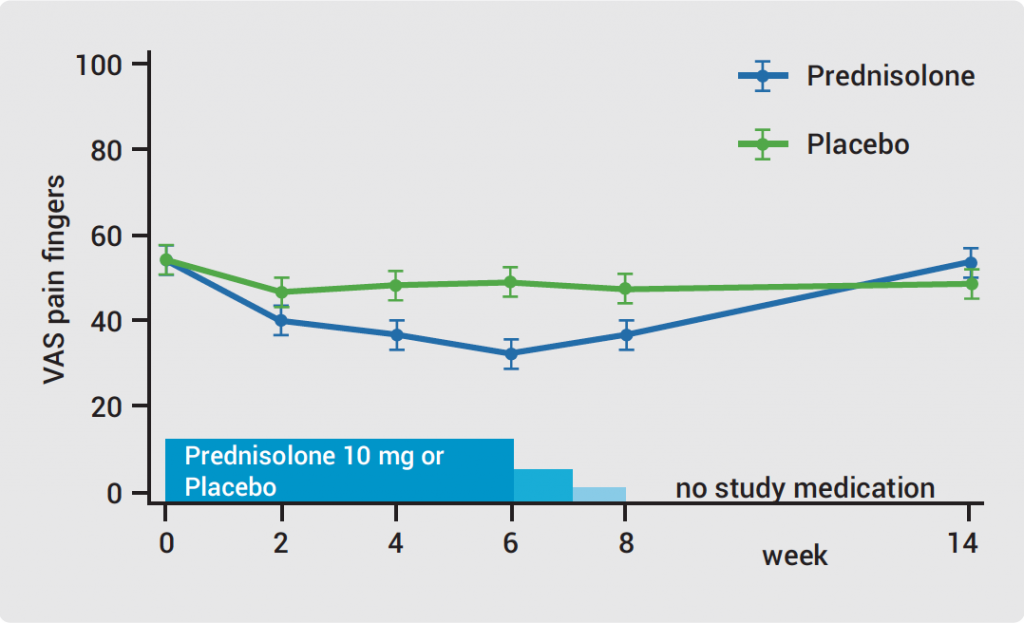
Hand OA: low-dose corticosteroids improve symptoms
September 4, 2019
What is new in osteoarthritis
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

