https://doi.org/10.55788/a5d9a375
Insufficient data exists to guide the selection of therapy in the context of RA-ILD. As such, a study designed by Dr Bryant England (University of Nebraska Medical Center, NE, USA) and his colleagues aimed to compare survival and respiratory-related outcomes in patients with RA-ILD who initiate treatment with TNFi or non-TNFi biologic/JAKi. This American group set up an active-comparator, new-user study of patients in the Veterans Health Administration (VA) between 2006 and 2018. The primary outcome was a composite of time to respiratory-related hospitalisation or death after 3 years. Secondary outcomes included respiratory hospitalisation and death after 1 year, because by that time, many patients were expected to have already made treatment adjustments.
Of 1,046 eligible RA-ILD patients, 237 TNFi initiators were matched to 237 non-TNFi/JAKi initiators in the primary analyses. The mean age was 68 years, and 92% were male. The most frequently used TNFi were adalimumab (51%) and etanercept (37%), while rituximab (53%) and abatacept (28%) were the most frequent non-TNFi/JAKi.
An increased risk of death or respiratory hospitalisation among RA-ILD patients who initiate a TNFi was not observed. The number of events was 108 in the non-TNFi/JAKi group versus 98 in the TNFi group (HR 1.21; 95% CI 0.92–1.59). No significant differences in the secondary outcomes were observed between both groups concerning mortality at year 3 (HR 1.11; 95% CI 0.78–1.58), respiratory hospitalisation at year 3 (HR 1.27; 95% CI 0.92–1.76), composite of death or respiratory hospitalisation at year 1 (HR 1.41; 95% CI 0.93–2.13), mortality at year 1 (HR 1.25; 95% CI 0.68–2.32), and respiratory hospitalisation at year 1 (HR 1.53; 95% CI 0.95–2.48).
The authors concluded that their findings do not support the need to systematically avoid TNFi to treat RA-ILD. However, various issues require clarification to make a well-informed choice between TNFi and non-TNFi/JAKi for these patients. It is still unknown if TNFi are safe in specific types of RA-ILD or specific subpopulations. Importantly, the above findings do not clarify whether TNFi are efficacious in RA-ILD. Data comparing the safety and efficacy of different DMARDs are needed to guide treatment decisions further.
- England B, et al. Non-TNFi b/tsDMARDs vs. TNFi in rheumatoid arthritis-interstitial lung disease: An active-comparator, new-user, propensity score matched study using national veterans affairs data. 1582, ACR Convergence 2023, 10–15 November, San Diego, USA.
Medical writing support was provided by Michiel Tent.
Copyright ©2023 Medicom Medical Publishers
Posted on
Previous Article
« Baricitinib superior to TNFi in patients with RA who failed csDMARDs Next Article
Reduced-dose glucocorticoids in GPA and MPA increase mortality »
« Baricitinib superior to TNFi in patients with RA who failed csDMARDs Next Article
Reduced-dose glucocorticoids in GPA and MPA increase mortality »
Table of Contents: ACR 2023
Featured articles
Ixekizumab resolves nail psoriasis better than adalimumab in PsA
IV secukinumab safe and effective for long-term treatment of active PsA
Rheumatoid Arthritis
Short-term glucocorticoid use increases the risk of MACE
Positive efficacy and safety results of novel BlyS/APRIL inhibitor in RA
Baricitinib superior to TNFi in patients with RA who failed csDMARDs
Lupus
Encouraging results of afimetoran in participants with cutaneous lupus
CAR-T cell therapy results in sustained lupus remission
Osteoarthritis
Repeat steroid injection in knee osteoarthritis possibly beneficial
Osteoporosis
Romosozumab tops denosumab in glucocorticoid users with high fracture risk
Psoriatic Arthritis
Ixekizumab resolves nail psoriasis better than adalimumab in PsA
IV secukinumab safe and effective for long-term treatment of active PsA
Apremilast in early oligoarticular PsA: phase 4 study results
Gout
Novel selective URAT1 inhibitor shows promise in gout
Fibrosing rheumatic diseases
Incidence and risk factors for new-onset interstitial lung disease
No need to avoid TNF inhibitors in RA-ILD?
Vasculitis
Reduced-dose glucocorticoids in GPA and MPA increase mortality
Related Articles
August 14, 2020
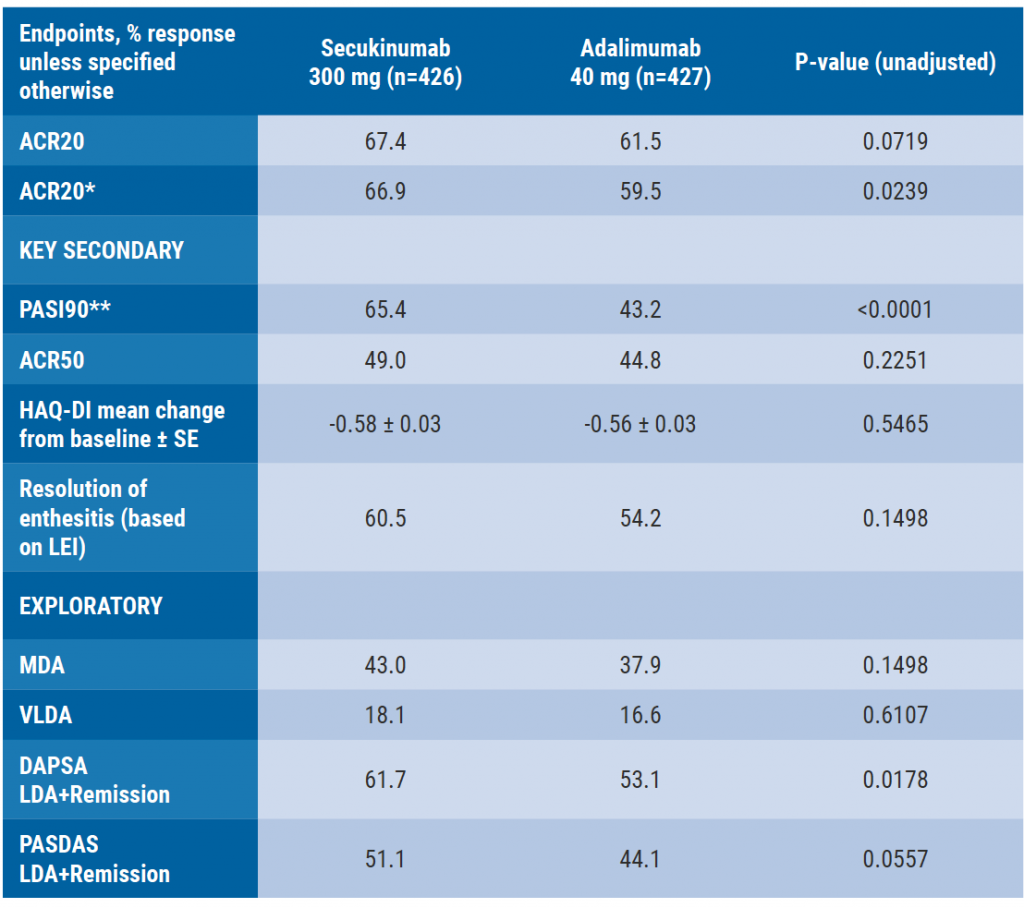
Secukinumab monotherapy as efficient as adalimumab

September 4, 2019
Ixekizumab improves signs and symptoms in TNFi-naïve PsA patients
January 18, 2021
No progression of osteoarthritis with corticosteroid injections
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

