Phase 3 clinical trials of all 3 COVID-19 vaccines excluded patients on immunosuppressants or immune-modifying drugs within 6 months of enrolment, so there is little data on the immunogenicity of SLE patients. “Many of us in the rheumatology community have been working on addressing the question of whether certain immunosuppressive medications affect the response to the new COVID-19 vaccines,” said Dr Peter Izmirly (New York University Grossman School of Medicine, NY, USA). This is particularly important because some people with lupus have been hesitant about getting vaccinated for fear of a disease flare. “Our group has previously shown that after natural infection with SARS-CoV-2, most lupus patients developed and maintained a serologic response to the virus,” Dr Izmirly explained.
The current study explored the serological response and the development of SLE flares among a group of a multi-ethnic/racial SLE patient cohort (n=90) compared with 20 healthy controls after COVID-19 vaccination [1]. “We decided to limit our study to only patients with SLE to assess both the medications and disease effect on the response to the vaccine and to assess any change in disease activity post-vaccination.”
All patients in the study received a complete COVID-19 vaccine schedule. IgG seroreactivity to the SARS-CoV-2 spike receptor-binding domain and SARS-CoV-2 microneutralisation were used to evaluate B-cell response to the vaccine, while T-cell response was assessed by ELISpot through IFN-gamma production.
In general, patients with SLE had lower mean antibody titres after vaccination compared with healthy patients. Researchers found that 26 (29%) SLE patients developed an IgG antibody response to the SARS-CoV-2 spike receptor-binding domain, which fell below the lowest response obtained for the controls. In bivariate analysis, lower vaccine response was associated with the use of prednisone or immunosuppressants. In contrast, taking anti-malarial drugs was associated with a more positive response to the vaccine. In addition, having normal anti-dsDNA antibodies before vaccination was associated with a low vaccine response (see Table). An analysis including only those patients who were on any immunosuppressants confirmed the association of a normal anti-dsDNA antibody with poor response.
Table: Predictors for low vaccine response in SLE patients in a logistic regression analysis [1]

Regarding disease activity, there were no meaningful differences in SLEDAI scores between pre-vaccine and post-vaccine visits. Only 11% of patients experienced disease flares after vaccination, 1% of them severe. “The data from our group and others has shown that overall disease activity did not change after vaccination. Our study also showed that severe flares were rare. Most flares were mild to moderate and manageable,” Dr Izmirly commented. A limitation of this study is that vaccine efficacy threshold levels are not yet established.
Certain medications or combinations of medications could affect the efficacy of the vaccines. While minimal protective levels remain unknown, these data suggest protocol development is needed to assess the efficacy of booster vaccination. The rare occurrence of severe flares supports the relative safety of vaccination in SLE patients.
- Izmirly PM, et al. Evaluation of Immune Response and Disease Status in SLE Patients Following SARS-CoV-2 Vaccination. Abstract 1420, ACR Convergence 2021, 03–10 November.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Promising results in uric acid-lowering in gout patients with a new xanthine oxidase inhibitor Next Article
Sequential rituximab after belimumab does not improve disease control in SLE »
« Promising results in uric acid-lowering in gout patients with a new xanthine oxidase inhibitor Next Article
Sequential rituximab after belimumab does not improve disease control in SLE »
Table of Contents: ACR 2021
Featured articles
Late-Breaking Abstracts
Vaccine booster improves immune response in patients treated with rituximab
IL-17 inhibition showing efficacy in GCA in phase 2 trials
Spotlight on Rheumatoid Arthritis
Cycling JAK inhibitors shows similar effectiveness to switching to a bDMARD in difficult-to-treat RA
Pre-existing heart failure affects safety of hydroxychloroquine in RA patients
Patients with RA-associated interstitial lung disease benefit from antifibrotic agent
Ultra-low dosing of rituximab in RA is a viable treatment option
Kidney disease and hydroxychloroquine dose are risk factors for developing retinopathy
More pros than cons for the use of statins in RA
Psoriatic Arthritis: Novel Developments
Selective IL-23 inhibition: a new option in active PsA
Ustekinumab: highly efficacious in PSA independent of methotrexate
COVID-19: What You Need to Know
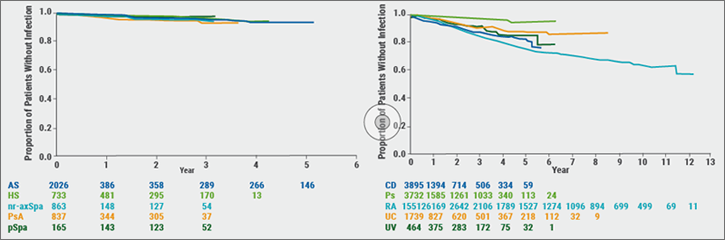
Vaccinated rheumatic patients carry increased risk for COVID-19 breakthrough infections
B-cell depleting medication increases COVID-19 breakthrough infection outcome risk
COVID-19 mRNA vaccine safe and tolerable in adults with autoimmune disease
SLE Treatment: What Is New
Iberdomide: an upcoming new treatment possibility in lupus erythematosus
Sequential rituximab after belimumab does not improve disease control in SLE
Lupus patients less protected by COVID-19 vaccine
Late-Breaking Posters
Promising results in uric acid-lowering in gout patients with a new xanthine oxidase inhibitor
Laboratory and clinical signs 24h after hospitalisation predict MIS-C in children
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy