More and more JAK inhibitors are entering the therapeutic arena.* Therefore, it is possible to use a second JAK inhibitor if the first JAK inhibitor fails in patients with RA. “In real life, JAK inhibitors are being used primarily in patients who have already failed treatment with a biologic disease-modifying antirheumatic drug (bDMARD), and they have shown to be effective in these situations,” Dr Manuel Pombo-Suarez (Hospital Clinico Universitario de Santiago De Compostela, Spain) explained. “Looking at the 2020 update of the EULAR management recommendations for patients with RA who have failed a biologic DMARD or first JAK inhibitor, recommendation is that treatment with another biologic or another JAK inhibitor should be considered” [1]. At the time of the publication, no study data was available on the use of a second JAK inhibitor after failure/intolerance of a first JAK inhibitor. The rationale for the JAK-pot study was to investigate the efficacy of cycling from one JAK inhibitor to a second and to compare this with the efficacy of switching from a JAK inhibitor to a biologic [2].
This nested cohort study included prospectively collected data on 708 RA patients (data obtained from 14 national registries of the JAK-pot collaboration) who failed a first JAK inhibitor and were then treated with either a second JAK inhibitor (cycling) or a bDMARD (switching) in routine care. A total of 154 patients cycled and 554 switched. The researchers compared the effectiveness of both treatment strategies on drug retention and disease activity, measured by DAS28 disease activity scores, over 1 year after they started their second treatment. Patients cycling JAK were older, had RA for longer, had already received more bDMARDs, and had longer exposure to the first JAK inhibitor than those who switched. Monotherapy was more common, and discontinuation of the first JAK inhibitor was more common for safety reasons than lack of efficacy. “JAK inhibitor cyclers had a more difficult treatment profile than the others,” Dr Pombo-Suarez commented.
After 2 years of follow-up, cycling and switching showed similar drug survival. However, the researchers noted an interesting, although not statistically significant, trend: patients who cycled were more likely to discontinue the second treatment when they originally stopped their first JAK inhibitor because of side effects rather than lack of efficacy.
Over time, DAS28 improved similarly in both the cycling and switching groups after 1 year. “This was precisely the goal of our study: to refine treatment options after failure/intolerance to a JAK inhibitor. We intend to provide an answer for a growing population of RA patients who have failed treatment to JAK inhibitors,” said Dr Pombo-Suarez. “A limitation of our study is that most patients received tofacitinib. It will be interesting to see new JAK inhibitors included in the future,” he said. The most important take-away is that the effectiveness of cycling to another JAK inhibitor is no different from that of switching to a bDMARD. “Cycling JAK inhibitors is kind of a desperate scenario, but this might change in the future,” Dr Pombo-Suarez concluded.
- Smolen JS, et al. Ann Rheum Dis 2020;79:685-99.
- Pombo-Suarez M, et al. Effectiveness of Cycling JAKi Compared to Switching to bDMARD in patients who failed a first JAKi in an international collaboration of registries of rheumatoid arthritis patients (the JAK-pot Study). Abstract 1442, ACR Convergence 2021, 3–10 November.
*In September, the FDA announced a safety concern regarding the use of JAK inhibitors: Based on a completed FDA review of a large, randomised safety clinical trial, the FDA concludes that there is an increased risk of serious heart-related events such as heart attack or stroke, cancer, blood clots, and death with the use of tofacitinib. In contrast to an earlier evaluation, an increased risk of blood clots and death has also been reported with the lower dose of tofacitinib. The FDA also requires new and updated warnings for baricitinib and upadacitinib. The risks of these agents has not been adequately evaluated, but since they share the same mechanism of action, FDA considers that these medicines may have similar risks (for more information, see https://www.fda.gov/drugs/drug-safety-and-availability/fda-requires-warnings-about-increased-risk-serious-heart-related-events-cancer-blood-clots-and-death).
Copyright ©2022 Medicom Medical Publishers
Posted on
« Pre-existing heart failure affects safety of hydroxychloroquine in RA patients Next Article
IL-17 inhibition showing efficacy in GCA in phase 2 trials »
Table of Contents: ACR 2021
Featured articles
Late-Breaking Abstracts
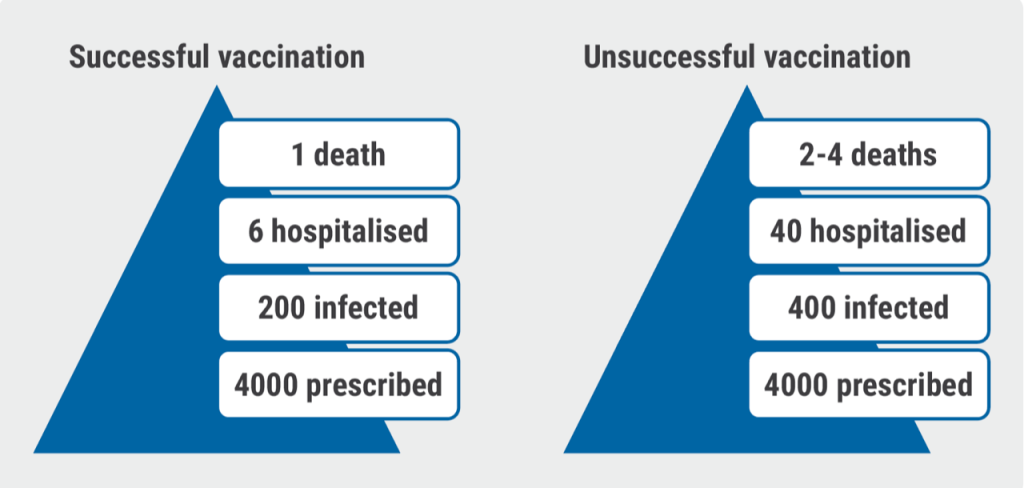
Vaccine booster improves immune response in patients treated with rituximab
IL-17 inhibition showing efficacy in GCA in phase 2 trials
Spotlight on Rheumatoid Arthritis
Cycling JAK inhibitors shows similar effectiveness to switching to a bDMARD in difficult-to-treat RA
Pre-existing heart failure affects safety of hydroxychloroquine in RA patients
Patients with RA-associated interstitial lung disease benefit from antifibrotic agent
Ultra-low dosing of rituximab in RA is a viable treatment option
Kidney disease and hydroxychloroquine dose are risk factors for developing retinopathy
More pros than cons for the use of statins in RA
Psoriatic Arthritis: Novel Developments
Selective IL-23 inhibition: a new option in active PsA
Ustekinumab: highly efficacious in PSA independent of methotrexate
COVID-19: What You Need to Know
Vaccinated rheumatic patients carry increased risk for COVID-19 breakthrough infections
B-cell depleting medication increases COVID-19 breakthrough infection outcome risk
COVID-19 mRNA vaccine safe and tolerable in adults with autoimmune disease
SLE Treatment: What Is New
Iberdomide: an upcoming new treatment possibility in lupus erythematosus
Sequential rituximab after belimumab does not improve disease control in SLE
Lupus patients less protected by COVID-19 vaccine
Late-Breaking Posters
Promising results in uric acid-lowering in gout patients with a new xanthine oxidase inhibitor
Laboratory and clinical signs 24h after hospitalisation predict MIS-C in children
Related Articles
Rivaroxaban cuts blood clot risk after COVID-19 hospital discharge
COVID-19 has disrupted cancer care, particularly among minority groups
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

