A rapid and accurate diagnosis of COVID-19 is essential, but symptoms are numerous and non-specific. Recently, concerns have been raised about the performance and real-life sensitivity of SARS-CoV-2 PCR testing. The interpretation of a negative PCR test can be difficult, as a negative result does not rule out the presence of the virus. Therefore, Dr Thomas Gille (Université Paris 13, France) and colleagues aimed to determine the clinical, biological, and radiological characteristics of patients with a false-negative first PCR test, but a final diagnosis of COVID-19 [1,2]. A secondary aim was to assess the outcome of these COVID-19 patients with a first negative PCR.
This retrospective, multicentre, case-control study was conducted in patients admitted to 11 hospitals in France and Belgium. Patients were included between 30 March 2020 and 22 June 2020. Adult patients were included when hospitalised for COVID-19. Exclusion criteria were pneumonia with another causative agent, pregnancy, recent delivery, lactation, and guardianship.
In total, 138 patients were included in France, and 22 in Belgium. Of these patients, 80 PCR-negative cases were matched to 80 controls with a positive first PCR on age, sex, and initial admission unit (wards vs intensive care unit). Data was collected on demographics, symptoms, lab tests, thoracic CT scan findings, treatments, need and duration of mechanical ventilation, and outcome of discharge. Multiple logistic regression was used to analyse the data.
The final diagnosis of COVID-19 (n=80) was based on a thoracic CT scan in most patients (n=71, 89%), followed by a contagion history (n=15, 19%), subsequent positive PCR tests (n=11, 14%), and serological testing (n=2, 3%). Demographics and baseline characteristics did not differ between cases and controls. PCR tests were done after a median of 6 days in cases and 5 days in controls (P=0.27). Mortality, hospital length-of-stay, need for antiviral medication, and mechanical ventilation did not differ between the groups. Patients with platelet counts >207x103/mm3 and/or CRP levels >79.8 mg/L were at increased risk of having a false-negative first PCR test (aOR 3.81, P=0.034; aOR 4.00, P=0.023, respectively; see Figure). Moreover, patients with non-specific symptoms as fatigue or headache had a lower risk of false-negative first PCR. The time between symptom onset and PCR test was not associated with test positivity.
Figure: Predictive factors of false-negative PCR [1]
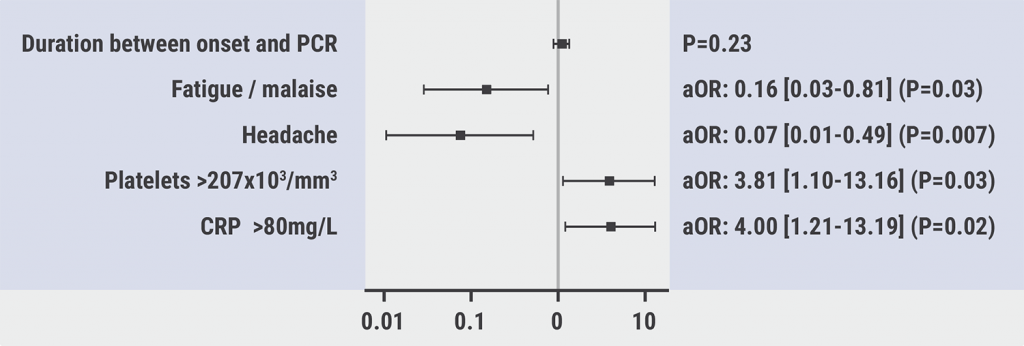
In conclusion, patients with higher inflammation markers were at increased risk of false-negative first PCR. Patients with suspected COVID-19 but a negative first PCR test should be repeatedly tested by PCR. Alternatively, a CT scan should be used for diagnosis.
- Gille T, et al. Predictors of negative first SARS-CoV-2 PCR despite final diagnosis of COVID-19 and association with outcome. Abstract 2662, ERS 2021, 5–8 September.
- Lascarrou JB, et al. Sci Rep 2021;11(1):1–7.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Breathing techniques contributed to COVID-19 recovery Next Article
Letter from the Editor »
« Breathing techniques contributed to COVID-19 recovery Next Article
Letter from the Editor »
Table of Contents: ERS 2021
Featured articles
Letter from the Editor
COVID-19 Research: Looking Back and Moving Forward
Higher inflammation markers in COVID-19 patients with a first negative PCR test
Persistent fatigue following COVID-19
Risk of COVID-19-related morbidity and mortality in young and middle-aged adults
Respiratory Viral Infections: Insights from Recent Studies
Rhinovirus bronchiolitis increased risk of recurrent wheezing and asthma
COPD: Evidence Update
Livestock farming affected the airway microbiome of COPD patients
Reduction of COPD severe acute exacerbations by candidate vaccine
Paediatrics and Vaccinology
Better lung function in children with a healthy diet
Need for validated severity score in the assessment of bronchiolitis
Increased impact of air pollution on lung function in preterm infants
Pearls in Asthma Research
Biomarkers do not discriminate severe from severe uncontrolled asthma
Increased blood neutrophiles in patients with obesity and asthma
Blood inflammatory phenotypes associated with clinical symptoms of asthma
Related Articles
October 30, 2022
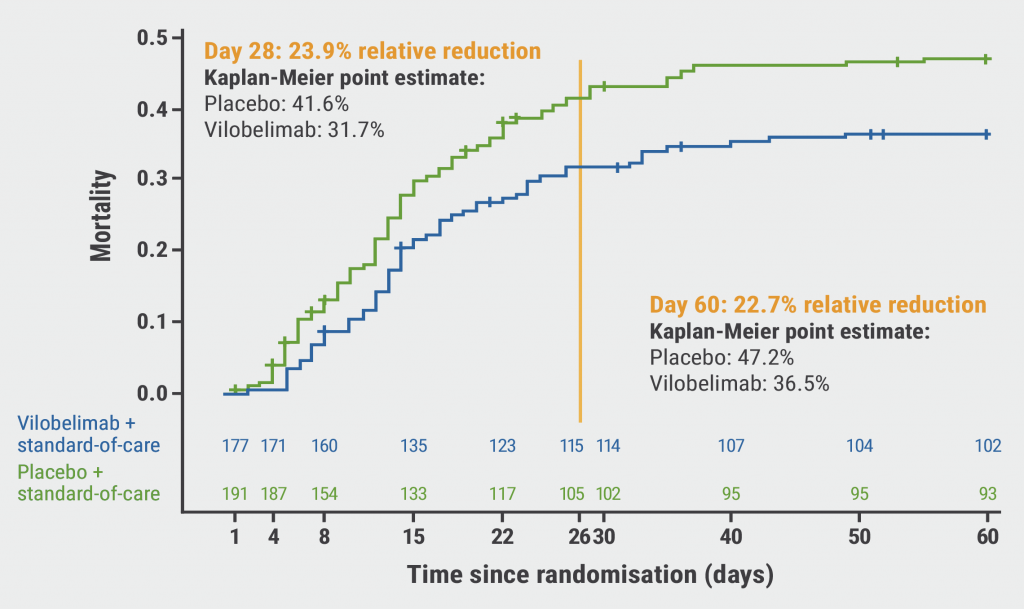
Does vilobelimab reduce mortality in severe COVID-19?
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

