Previous studies have shown associations between dietary patterns and lung function in adults. For example, the Mediterranean diet has been associated with beneficial health effects. However, data on the relationship of food and lung function in children is scarce. Lung function in childhood is particularly important, because in childhood maximum lung function is being developed which has a life-long impact. Dietary patterns are the combined effects of all foods consumed. Two main approaches for characterising dietary patterns are commonly used: empirical methods and a priori indices. Dr Mohammad Talaei Pashiri (Queen Mary University of London, UK) and his team investigated whether 3 distinct dietary patterns in mid-childhood were associated with lung function in adolescence in the longitudinal ALSPAC study [1].
A birth cohort in Bristol, UK, was used for the current analysis. The study identified 3 dietary patterns: ‘junk’, ‘traditional’, and ‘health-conscious’. Junk food was a synonym for processed food, including white bread, sweets, cakes, ice cream, and chocolate, among others. Traditional food included poultry, red meat, vegetables, fish, and rice. Health-conscious food had overlap with traditional food regarding fish, vegetables, and rice, but also included vegetarian options, nuts, and fruit. Parents were asked to fill out food frequency questionnaires when their child reached the age of 7 years. At 15.5 years of age, lung function was measured.
The primary outcome was lung function measurements transformed to z-scores based on the Global Lung Function Initiative (GLI) curves. The primary outcome was adjusted for age, height, ethnicity, and sex. Multivariable linear regression analysis was performed and the model was adjusted for potential confounders, including demographics, urban/rural, parental history of atopic disease, maternal smoking, siblings, physical activity, and total energy intake. In addition, potential mediators were considered, including vitamins, minerals, and adiposity.
In total, 14,541 mothers were asked to participate in the original study. Of these mothers, 8,035 completed diet data. Around 3,500 lung function assessments were done. Post-bronchodilator lung function measures were done in 3,085 children. In the participating children, the health-conscious pattern was associated with higher FVC (P=0.006) and FEV1 levels (P=0.02; see Table). Conversely, the junk food pattern was associated with significant lower levels of FVC (P=0.009) and FEV1 (P=0.04).
Table: Linear regression coefficients for lung function measures (z scores) according to quartiles of dietary pattern scores, adjusted for potential confounders [1]
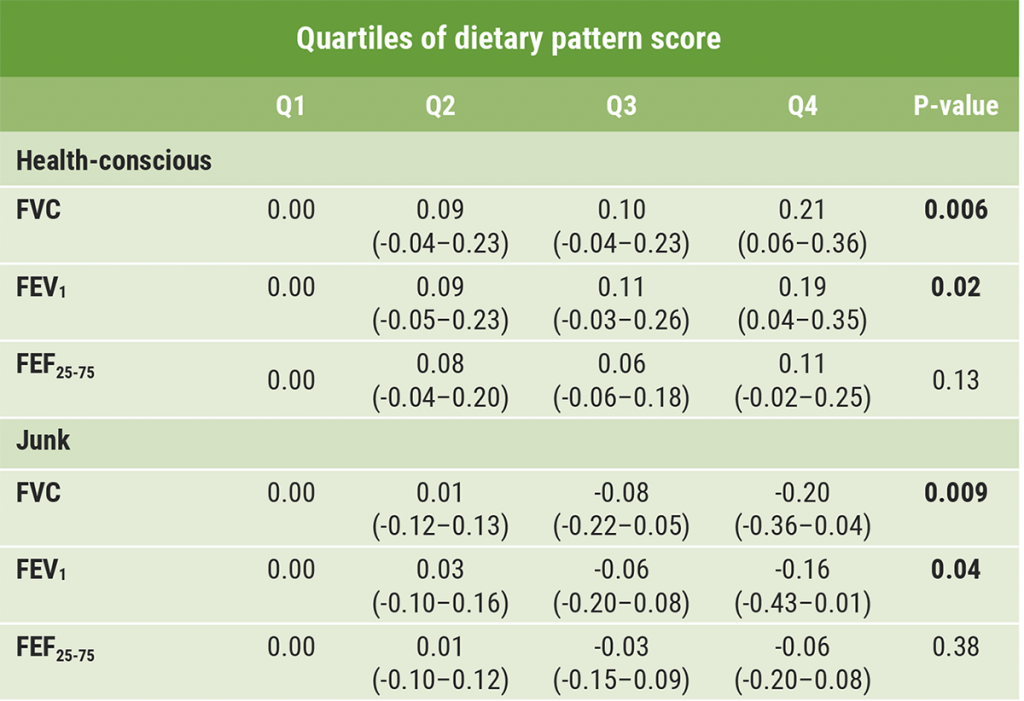
Significant P-values in bold.
No association was found for traditional dietary pattern and lung function. In addition, no effect of mediation was found for vitamins, minerals, and adiposity. However, zinc partially explained the negative association between the junk food pattern and FVC.
In conclusion, a healthier diet was associated with higher subsequent lung function, while a diet high in processed food was associated with lower lung function.
- Talaei Pashiri M, et al. Dietary patterns and lung function in childhood: A longitudinal study. Abstract 2960. ERS 2021, 5–8 September.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Impaired response to pneumococcal vaccine in children with recurrent respiratory infections Next Article
Lower influenza vaccination coverage in children with chronic conditions »
« Impaired response to pneumococcal vaccine in children with recurrent respiratory infections Next Article
Lower influenza vaccination coverage in children with chronic conditions »
Table of Contents: ERS 2021
Featured articles
Letter from the Editor
COVID-19 Research: Looking Back and Moving Forward
Higher inflammation markers in COVID-19 patients with a first negative PCR test
Persistent fatigue following COVID-19
Risk of COVID-19-related morbidity and mortality in young and middle-aged adults
Respiratory Viral Infections: Insights from Recent Studies
Rhinovirus bronchiolitis increased risk of recurrent wheezing and asthma
COPD: Evidence Update
Livestock farming affected the airway microbiome of COPD patients
Reduction of COPD severe acute exacerbations by candidate vaccine
Paediatrics and Vaccinology
Better lung function in children with a healthy diet
Need for validated severity score in the assessment of bronchiolitis
Increased impact of air pollution on lung function in preterm infants
Pearls in Asthma Research
Biomarkers do not discriminate severe from severe uncontrolled asthma
Increased blood neutrophiles in patients with obesity and asthma
Blood inflammatory phenotypes associated with clinical symptoms of asthma
Related Articles
July 23, 2019
Human lung organoids to study foetal RSV infection
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

