Despite the fact that HER2-directed therapies like trastuzumab, pertuzumab, and T-DM1 have led to improved outcomes for patients with HER2-positive advanced breast cancer, resistance to these drugs is almost inevitable. Once patients develop resistance, it is not clear what treatment should be given, highlighting the unmet medical need for new and improved therapies for these patients. T-DXd is an antibody-drug conjugate with an HER2 antibody, peptide-based cleavable linker, and a novel topoisomerase I inhibitor payload. In a phase 1 trial, it has shown to yield an objective response rate of 59% in patients with advanced HER2-positive breast cancer who were previously treated with T-DM1 [1]. Krop et al. conducted a phase 2 study in which 253 patients with metastatic HER2-positive breast cancer previously treated with T-DM1 were included [2]. Median age of the patients was 55 years, 34.2% was Asian, 28.8% North American, and 37% European; 52.7% was HER2+ and 45.1% was HER2- (of 2.2% of patients, the HER2 status was unknown). The median prior lines of cancer therapy was 6 (range 2-27). The trial consisted of 3 parts, I, IIa, and IIb. In total, 184 patients received the recommended phase 2 dose of 5.4 mg/kg T-DXd. Median treatment duration was 6.9 months.
The results showed that the overall response rate (ORR) was 60.9%, and that 6% had a complete response versus 54.9% with a partial response (see Table). The median progression-free survival was 16.4 months (95% CI 12.7-NE). Median overall survival was not reached.
Table. Primary endpoint: ORR in the intention-to-treat population (n=184) [2]
 ORR, overall response rate; ICR, independent central review
ORR, overall response rate; ICR, independent central reviewTreatment-emergent adverse events (AEs) occurred in 99% of patients of which 51% were grade ≥3. The most common any-grade treatment-emergent AEs were gastrointestinal AEs such as nausea (77%), vomiting (45%), constipation (34%), decreased appetite (29%), and diarrhoea (27%). Other treatment-emergent AEs were alopecia (48%) and fatigue (48%). The most common grade ≥3 AEs were decreased neutrophil count (17%), nausea (7.6%), anaemia (6.5%), decreased lymphocyte count (5.4%), and fatigue (5.4%).
Noteworthy, ILD of any grade occurred in 13.6% of patients; 2.7% of cases was grade 1, 8.2% was grade 2, 0.3% was grade 3, 0% was grade 4, and 2.2% was grade 5. Of these total 25 events, the mean time to investigator-reported onset was 193 days (range 43-535 days); 7 patients recovered, 2 were recovering, 12 were either outcome unknown or not followed until resolution, and 4 patients died. Of these 4 fatal cases, onset of ILD was from 63-148 days, 3 patients received steroids as part of the treatment, and death occurred 9-60 days after diagnosis of ILD. Researchers recommend to monitor patients for symptoms, hold T-DXd, and start steroids as soon as ILD is suspected [2].
1. Tamura K, et al. Lancet Oncol. 2019;20(6);816-826.
2. Krop IA, et al. GS1-03. SABCS 2019.
Posted on
Previous Article
« Partial breast irradiation could be as effective as whole breast irradiation Next Article
Neoadjuvant + adjuvant pembrolizumab improves pCR in triple-negative breast cancer with lymph node involvement »
« Partial breast irradiation could be as effective as whole breast irradiation Next Article
Neoadjuvant + adjuvant pembrolizumab improves pCR in triple-negative breast cancer with lymph node involvement »
Table of Contents: SABCS 2019
Featured articles
Screening, Detection, and Diagnosis
Phase 2 Trial Update
Phase 3 Trial Update
Long-Term Study Results
Triple-Negative Breast Cancer
HER2-Positive Breast Cancer
Related Articles
February 13, 2020
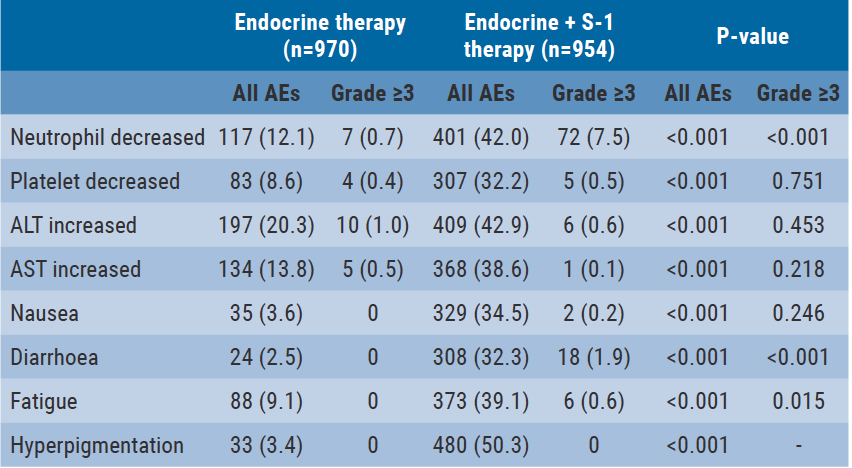
S-1 shows promising results in combination with endocrine therapy
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

