"Although TORS has gained widespread adoption as a surgical technique, selecting which patients can benefit the most from TORS has been a moving target," Dr. Robert Brody of Penn Medicine in Philadelphia told Reuters Health by email. "While older patients may try to avoid surgery when possible, radiotherapy and chemotherapy have been shown to be more toxic in older populations."
"Clinicians caring for older patients diagnosed with oropharyngeal cancer should know that TORS in carefully selected patients can result in excellent outcomes, similar to those in younger patients," he said. "Moreover, ...greater than one-third of patients were able to undergo surgery alone without the side effects of radiation or chemotherapy."
"Many patients who received post-operative radiotherapy were given decreased doses of radiation," he added, "thus limiting the costs and side effects associated with treatment."
In JAMA Otolaryngology-Head and Neck Surgery, Dr. Brody and colleagues report on 77 HPV-associated oropharyngeal cancer patients treated from 2010-2017. The median age at diagnosis was 73, and 75% were men. The median follow-up was 39.6 months.
Perioperative mortality was 1.3% (one death within 30 days of surgery) and the rate of oropharyngeal hemorrhage was 2.6%.
Thirty-nine percent of patients avoided all adjuvant therapy, as Dr. Brody noted, whereas 74% avoided chemotherapy. Specifically, 27 patients (35.1%) underwent postoperative radiotherapy and 20 (26%) had postoperative chemoradiotherapy.
Three-year survival estimates were 92.4% for disease-specific survival (DSS), 90% for overall survival (OS), and 84.3% for disease-free survival (DFS).
On univariate analysis, OS was negatively impacted by increasing age (hazard ratio, 1.18); however, DFS and DSS were not. However, DFS (HR, 5.27) and DSS (HR, 6.99) were lower in patients with stage II versus stage I disease and other negative pathologic indicators (lymphovascular invasion, perineural invasion, and extranodal extension).
Multivariable analyses could not be done because the events of interest were too infrequent to reach minimum statistical thresholds.
Regarding limitations, the authors note that in addition to the retrospective/observational design of the study, "our cohort underwent TORS, neck dissection, and adjuvant therapy as indicated at a high volume and experienced center and there was no comparative conventional radiation therapy cohort, which may limit the generalizability of this study."
Dr. Thomas Gernon, a head and neck surgeon at City of Hope in Duarte, California, commented in an email to Reuters Health, "This approach is definitely beneficial to any patient population. Transoral robotic surgery offers the potential of treatment de-escalation and can offer a potential cure without the need for the possible side effects of chemotherapy and radiation."
That said, he noted, "Not all oropharynx tumors are candidates for transoral robotic surgery," and patients should be evaluated at major cancer centers by head and neck surgeons with fellowship training in transoral robotic surgery.
"Very advanced tumors that will be technically difficult to remove or that will functionally leave the patient in poor condition may not be candidates for surgical resection," he said.
By Marilynn Larkin
SOURCE: https://bit.ly/35gg0aa JAMA Otolaryngology-Head and Neck Surgery, online October 29, 2020.
Posted on
Previous Article
« ‘Reassuring’ data on cardiac toxicity with hydroxychloroquine in RA, lupus Next Article
Moderate-to-severe CKD tied to worse VTE outcomes »
« ‘Reassuring’ data on cardiac toxicity with hydroxychloroquine in RA, lupus Next Article
Moderate-to-severe CKD tied to worse VTE outcomes »
Related Articles
November 15, 2022
A Novel Microbiome Signature in Gastric Cancer
March 17, 2023
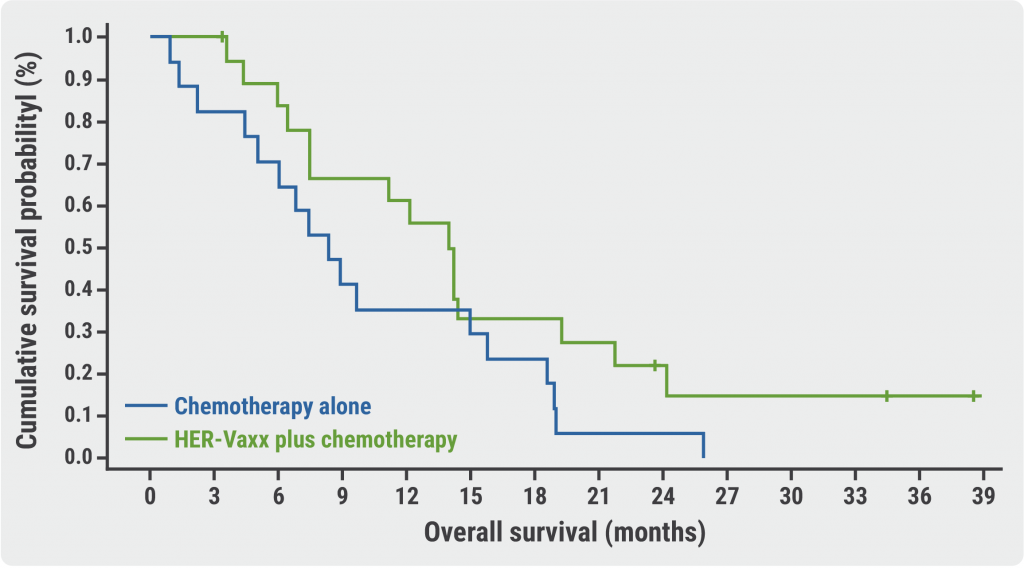
Promising phase 2 results for HER-Vaxx in gastric cancer
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

