https://doi.org/10.55788/58ee5330
The Neuromyelitis Optica Study Group (NEMOS) registry provides valuable real-world data on patients with MOGAD. Dr Vivien Häußler (University Medical Center Hamburg, Germany) and colleagues aimed to characterise clinical MOGAD phenotypes, identify risk factors for disease activity, and evaluate the current treatment strategies as well as the efficiency of the different immunotherapies [1].
The study cohort consisted of 248 patients with MOGAD who have been included in the NEMOS registry since 2016. The mean age at disease onset was 34.6 years and 59.7% were women. The mean follow-up was 7.3 years. Described phenotypes were optic neuritis in 46.8%, transverse myelitis in 24.6%, multiple symptoms in 16.9%, and other phenotypes in 11.3%. There were 138 patients (59%) with a relapsing disease course, while 95 (41%) had a single attack. On average, the relapsing group had a longer disease duration (10.6 vs 3.1 years; P<0.001) and a younger age (31.0 vs 39.9 years; P<0.001). After 160 weeks, half of the patients had relapsed; apart from time, an important risk factor for relapse was treatment: untreated patients had a higher risk of relapse than those who were treated at the time of the attack or before the attack (see Figure).
Figure: Impact of time (left) and treatment (right) on the risk of MOGAD relapse [1]

About half of all the patients (51%) received long-term immunotherapy. Over the last 10 years, the use of MS medication declined in this cohort. Azathioprine and rituximab were the most frequently prescribed therapies, the use of which remained stable; over the last 5 years, the use of tocilizumab has increased. The researchers only found a significant beneficial effect of rituximab plus classic immunosuppression (HR 0.17; 95% CI 0.04–0.82, P=0.028) and of tocilizumab (HR 0.09; 95% CI 0.02–0.49; P=0.005), compared with no treatment.
- Häußler V, et al. Clinical characteristics and immunotherapy in MOGAD patients: data from the NEMOS registry. O117, ECTRIMS 2024, 18–20 September, Copenhagen, Denmark.
Copyright ©2024 Medicom Medical Publishers
Posted on
Previous Article
« Improving skills of healthcare professionals in underserved areas for psoriasis Next Article
Comparative effectiveness and safety of DMTs in NMOSD »
« Improving skills of healthcare professionals in underserved areas for psoriasis Next Article
Comparative effectiveness and safety of DMTs in NMOSD »
Table of Contents: ECTRIMS 2024
Featured articles
Revised McDonald criteria allow earlier and more precise MS diagnosis
Approaches to RIS and MS converge
Diagnosis, Biomarkers, and Phenotypes
Revised McDonald criteria allow earlier and more precise MS diagnosis
Approaches to RIS and MS converge
AI versus clinicians: who diagnoses MS faster and better?
Blood markers predict MS progression
Gut microbiota modulate inflammation and cortical damage
Risk factors and importance of persistent PIRA
Vitamin D supplementation in progressive MS should be medically supervised
Treatment: Strategies
Encouraging real-world results of AHSCT to treat aggressive MS
CAR T-cell therapy in MS: in its infancy but highly anticipated
B cell-tailored dosing of ocrelizumab shows good results
First-line moderate-efficacy DMTs show similar efficacy
Treatment: Trials
Tolebrutinib slows disability worsening in relapsing MS
Frexalimab shows favourable safety and efficacy in OLE
Good safety of ozanimod over up to 8 years of treatment
Tolebrutinib slows disability in non-relapsing SPMS
High-dose simvastatin does not slow disability progression in SPMS
Pregnancy and Comorbidity Risks
Transfer of ocrelizumab into breastmilk is negligible
High genetic burden for depression associated with MS disease activity
More comorbidity is associated with worse clinical outcomes in MS
NMOSD/MOGAD
Ineffective response to EBV in MS not seen in similar diseases
Comparative effectiveness and safety of DMTs in NMOSD
Age, time, and treatment determine relapse risk in MOGAD
Related Articles
August 18, 2021
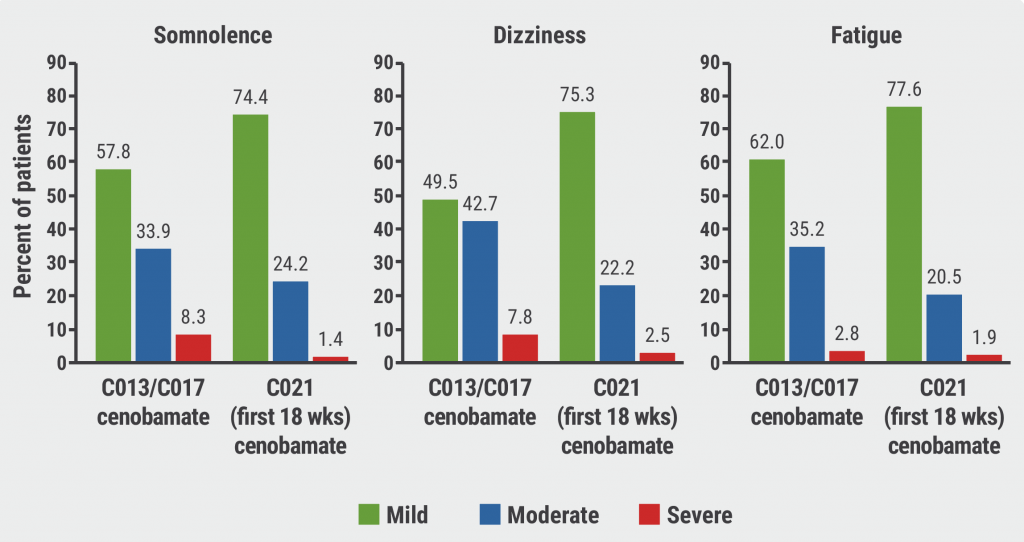
Good safety and efficacy of cenobamate for focal seizures
November 25, 2020
Anti-CD20 DMTs associated with worse COVID-19 outcomes
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

